Vol 28, No 4 (2025)
- Year: 2025
- Published: 01.11.2025
- Articles: 15
- URL: https://rjsvd.com/1560-9588/issue/view/9861
- DOI: https://doi.org/10.17816/dv.284
DERMATO-ONCOLOGY
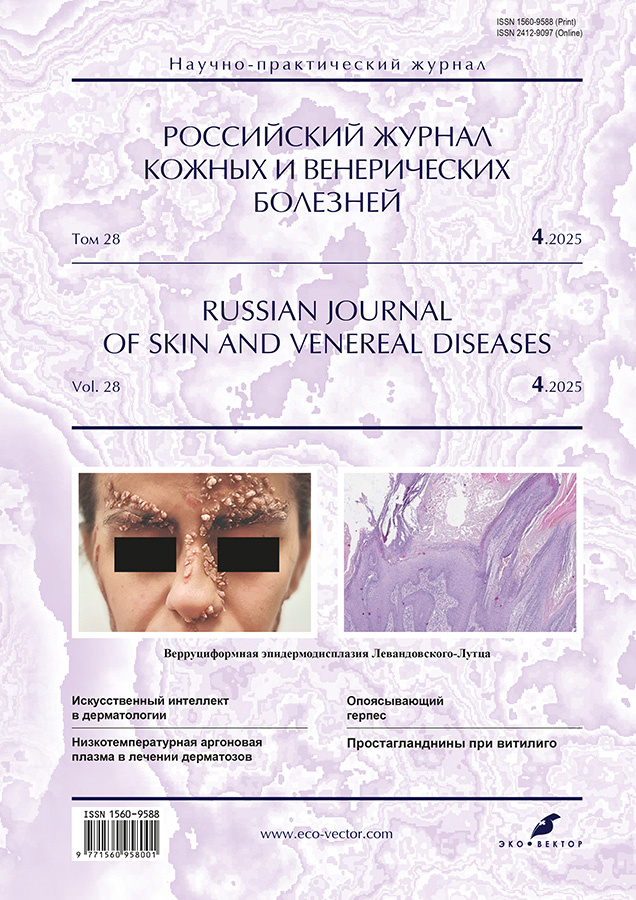
Lewandowsky–Lutz verruciform epidermodysplasia: a brief review and case report
Abstract
Verruciform (warty) epidermodysplasia (Lewandowsky–Lutz syndrome) is a rare autosomal recessive disease manifested by multiple cutaneous lesions associated with human papillomavirus infection. To date, no more than 500 patients with this form of genodermatosis have been reported worldwide. Hereditary forms of verruciform (warty) epidermodysplasia are caused by inactivating mutations in the TMC6, TMC8, CIB1, RHOH, and IL7 genes in a homozygous or compound heterozygous state. A non-classical variant of hereditary verruciform (warty) epidermodysplasia has also been described; it is associated with primary T-cell immunodeficiency resulting from mutations in the CORO1A, CARMIL2, DCLRE1C, DOCK8, ECM1, GATA2, LCK, MST1, RASGRP1, and TPP2 genes. Acquired verruciform (warty) epidermodysplasia usually develops in patients with secondary immunodeficiency of various origins.
The low prevalence and insufficient clinical diagnostic experience explain the lack of standardized therapy protocols and clinical guidelines for verruciform (warty) epidermodysplasia. Several researchers and clinicians have reported treatment of this condition using chemotherapeutic agents, immunomodulators, interferons, retinoids, and other drugs in combination with surgical excision or physical methods of lesion destruction.
This article presents a case report of aggressive verruciform (warty) epidermodysplasia without preceding immunodeficiency or alterations in key genes, describing the experience of treating the patient with a retinoid in combination with CO2 laser destruction of cutaneous lesions.
 369-380
369-380


Dermatoscopic methods for diagnosing radiation-induced skin reactions in patients with primary cutaneous lymphomas undergoing total skin electron beam therapy
Abstract
Background: Timely diagnosis and assessment of radiation-induced skin reactions remain an important challenge in modern medicine. Imaging techniques can help standardize the clinical evaluation of radiation dermatitis.
Aim: The work aimed to evaluate dermatoscopic features and confocal microscopy findings in radiation dermatitis among patients with primary cutaneous lymphomas undergoing radiotherapy, with subsequent analysis of the clinical and morphological characteristics of affected skin areas before treatment and at cumulative doses of 6 Gy, 14 Gy, and 30 Gy, based on macroscopic and dermatoscopic imaging of radiation-induced skin reactions for further comparison.
Methods: Data from 40 patients at the Granov Russian Scientific Center for Radiology and Surgical Technologies receiving electron beam radiotherapy for primary cutaneous lymphomas were analyzed. As clinical symptoms of radiation-induced skin reactions developed, morphological changes in the affected areas were examined. Dermatoscopic evaluation of skin lesions was performed using a HYPERLINK "https://shop.heine-med.ru/catalog/dermatoskopy/?ysclid=m63jpoace3558532091"Heine Optotechnik (Germany) dermatoscope at tenfold magnification. Confocal spectroscopy was conducted using the VivaScope® 1500 medical device (MAVIG GmbH, Munich, Germany). Instrumental data underwent correlation analysis to identify statistical relationships between dermatoscopic parameters and the severity of radiation-induced skin reactions.
Results: Dermatoscopy revealed patterns characteristic of different stages of radiation-induced skin reactions: reticular vascular arrangements in the dermis, brown scaly elements, perifollicular pigmentation, and follicular plugs arranged in rosette-like patterns. Confocal microscopy of radiation dermatitis lesions identified non-stochastic skin changes, including exocytosis (55.3%), spongiosis (63.5%), disorganization of the epidermis (65%), and abnormally structured dermal papillae (85.4%). Low-contrast microvascular cells marking vascular dysfunction in the dermal vascular bed were a specific feature of radiation dermatitis observed regardless of severity.
Conclusion: Accurate assessment of skin damage severity can help optimize the management of patients undergoing radiotherapy for primary cutaneous lymphomas. These findings are promising for integrating instrumental evaluation methods into routine clinical practice for early detection of radiation-induced skin changes and predicting disease severity.
 381-390
381-390


DERMATOLOGY
Modern approaches to the treatment of psychosomatic disorders associated with chronic dermatoses: a review
Abstract
Most contemporary studies indicate a high prevalence of psychosomatic disorders in patients with dermatological conditions.
This article presents a systematic scientific data review of therapeutic approaches to psychosomatic disorders associated with chronic dermatoses. The review summarizes data from various studies analyzing psychosomatic aspects of psoriasis, acne, alopecia, lichen planus, and vitiligo, including stress-induced mechanisms of their development and progression, the impact of stigmatization on patients’ psycho-emotional state, as well as quality of life. Particular attention is given to nosogenic (secondary) and comorbid psychiatric disorders associated with the underlying dermatological condition, such as anxiety–depressive disorders, social phobia, and hypochondriacal reactions. The rationale for implementing comprehensive therapeutic strategies has been substantiated, including psychopharmacological interventions (selective serotonin reuptake inhibitors, atypical antipsychotics, anxiolytics), cognitive behavioral therapy, and psychoeducational programs. Multidisciplinary approaches to patient management are considered, integrating dermatological treatment with psychotherapeutic and psychopharmacological methods aimed at improving patients’ adaptation. The article also provides updated information on the treatment of chronic dermatoses.
The scientific data search was conducted in national and international scientific databases (PubMed, Scopus, MedLine, Embase, Cochrane, Russian State Library, Central Scientific Medical Library of I.M. Sechenov First Moscow State Medical University).
According to the scientific data analysis, psychosomatic disorders comorbid with dermatological diseases require timely detection and treatment. Modern approaches to the treatment of psychosomatic disorders associated with skin diseases involve comprehensive therapy encompassing both dermatological care and psychocorrectional components (psychotherapy and psychopharmacotherapy). Social support also plays an important role. The competent use of psychocorrectional methods in combination with traditional dermatological therapy significantly enhances overall treatment efficacy, improves patients’ quality of life, and reduces the frequency of exacerbations of chronic dermatoses.
 391-400
391-400


Possibilities of IPL technology application in the treatment of patients with acne: review and personal clinical experience
Abstract
High-energy methods for acne treatment, particularly intense pulsed light (IPL), are gaining increasing popularity in dermatology and esthetic medicine.
This review analyzes data on the use of IPL in acne therapy. A systematic search of scientific publications over the past 20 years was conducted, focusing on various IPL application strategies and their effects on the main pathogenic mechanisms of acne. The role of IPL in modulating the skin microbiome and immune response is noted. Evidence is presented confirming the effectiveness of IPL both as monotherapy and in combination with systemic and topical medications. The authors’ own clinical experience in using a combination treatment method for the papulopustular form of mild-to-moderate acne in 28 women aged 18 to 45 years, involving a fixed-dose combination drug (adapalene and benzoyl peroxide) along with phototherapy using broad-spectrum non-coherent light (wavelength range 400–1200 nm), demonstrated a significant reduction in the total dermatological symptom severity index by 82.8% and an improvement in the dermatology life quality index by 80.5%, indicating high efficacy and good tolerability of the therapy.
The conducted analytical research and clinical experience support the feasibility of combining IPL with systemic and topical therapies for acne treatment and underscore the need for further research aimed at optimizing acne therapy and developing standardized practical guidelines.
 401-414
401-414


Role of integrated hematological biomarkers of systemic inflammation in assessing the effectiveness of anticytokine therapy in patients with psoriasis
Abstract
Background: Integrated hematological indices are accessible, cost-effective, and objective parameters for monitoring psoriatic inflammation both in everyday clinical practice and scientific research.
Aim: The work aimed to study the effect of anticytokine therapy with an IL-17A inhibitor on NLR, PLR, MLR, SII, and SIRI indices in patients with psoriasis of varying severity.
Methods: All patients enrolled in the study had systemic inflammation indices (SIRI, MLR, NLR, SII, PLR, and AISI) calculated before treatment and 6 months after therapy with the IL-17A inhibitor (netakimab). The Psoriasis Area and Severity Index (PASI) was used to assess lesion area and severity of skin involvement.
Results: The main group included 77 patients with psoriasis: 33 women (42.9%) and 44 men (57.1%), mean age 41.3 ± 13.4 years, mean PASI 10.8 (3.2; 15.3). Of these, 58 patients (75.4%) had only cutaneous manifestations, and 19 (24.6%) had psoriatic arthritis. In accordance with the clinical guidelines of the Ministry of Health of the Russian Federation for the treatment of patients with psoriasis and psoriatic arthritis, a subgroup of patients receiving IL-17A inhibitor therapy was identified. Subgroup 1 included 20 patients with moderate-to-severe psoriasis, and subgroup 2 included 19 patients with psoriatic arthritis. The total observation period was 10 months. No adverse reactions or complications were observed. Almost complete skin clearance (PASI 75) was observed in all patients of the study group 6 months after initiation of therapy. Different diagnostic trends were observed during treatment with netakimab when analyzing SIRI, MLR, NLR, SII, PLR, and AISI in patients of both subgroups. In patients with psoriatic arthritis, MLR, NLR, and PLR indices showed no statistically significant changes during the treatment. SIRI demonstrated significant changes in both subgroups, whereas AISI was significant only in patients with moderate-to-severe psoriasis. The systemic inflammation index SII proved to be less sensitive and demonstrated changes only in patients with skin manifestations of psoriasis (p = 0.030).
Conclusion: Integrated hematological indices of systemic inflammation are promising tools for evaluating the effectiveness of anticytokine therapy in patients with severe psoriasis. NLR, MLR, SII, and AISI can be applied to evaluate the decrease in systemic inflammation exclusively during therapy in patients with cutaneous manifestations of psoriasis, whereas SIRI proved to be effective in both patients with cutaneous psoriasis and those with psoriatic arthritis.
 415-428
415-428


Application of artificial intelligence technologies in dermatology
Abstract
Dermatology represents a field of medicine with extensive potential for analyzing pathological changes directly in the lesion site, which is reflected in the widespread use of morphological studies for diagnosing skin diseases. With the rapid integration of artificial intelligence technologies into medicine, dermatology has once again become a promising area for the testing and implementation of neural network- and machine learning-based methods for practical medical applications.
This article provides a review of scientific publications reporting the use of artificial intelligence technologies in dermatology. For this purpose, 120 research studies published between 2020 and 2025 and indexed in the PubMed database were analyzed.
The analysis established that artificial intelligence technologies can be used for the differential diagnosis of malignant skin neoplasms. A large number of images is critical for developing artificial intelligence-based platforms for skin melanoma due to the high heterogeneity of both the clinical and morphological presentation of neoplasms. At the same time, in some cases, image augmentation processes may enhance the effectiveness of the developed methods. In addition to neoplasms, machine learning methods have been applied to develop differential diagnostic algorithms for chronic dermatologic conditions such as atopic dermatitis, psoriasis, alopecia areata, rosacea, and acne. Along with clinical applications, the use of artificial intelligence in dermatology education has also been reported.
At the same time, the use of artificial intelligence raises patients’ concerns regarding ethical issues as well as the accuracy of diagnostic and therapeutic strategies; therefore, patients currently view these technologies primarily as complementary to physicians' work.
 429-436
429-436


Retinoids in dermatology: from structure to clinical application
Abstract
Vitamin A belongs to the group of essential fat-soluble vitamins that are not synthesized in the human body and are supplied with food. The primary function of vitamin A metabolites is to regulate cell growth and differentiation during ontogenesis and in the postnatal period. The widespread use of retinoids in dermatology is attributed to their ability to regulate the growth activity and differentiation of keratinocytes and epithelial cells of the sweat and sebaceous glands.
To date, pharmaceutical companies continue to work on improving retinoid molecules to enhance their clinical efficacy and reduce the risk of adverse events. At the same time, the clinical era of retinoids is still at an early stage of development, with research in vitamin A biochemistry significantly outpacing the therapeutic applications of its derivatives.
This article focuses on the analysis of the structure, functioning, and biological significance of retinoic receptors in cellular signaling. It examines receptor mechanisms, including classification, mechanisms of interaction with ligand molecules, and factors influencing their activity. The main receptor groups, their molecular characteristics, and intracellular signaling mechanisms triggered by synthetic vitamin A derivatives are described in detail. Special attention is given to receptor activation and desensitization processes, which play a pivotal role in regulating physiological processes. The molecular mechanisms underlying receptor activity, including conformational changes, phosphorylation, and interactions with intracellular signaling proteins, are discussed.
 437-448
437-448


Effectiveness of low-temperature argon plasma in the treatment of dermatological diseases: a review
Abstract
This review systematically summarizes and critically analyzes current evidence on the use of low-temperature atmospheric plasma in dermatology, focusing on its multimodal mechanisms of action and clinical efficacy. Unlike previous studies that examined individual effects of plasma, this review provides an integrative perspective on low-temperature atmospheric plasma as a therapeutic platform combining antimicrobial, regenerative, and immunomodulatory properties. Special attention is given to the paradoxical selectivity of low-temperature atmospheric plasma—its ability to stimulate the regeneration of normal tissues and simultaneously inducing apoptosis in pathologically altered cells.
The article provides an analysis of clinical studies on the use of low-temperature atmospheric plasma in various dermatological conditions (psoriasis, acne, atopic dermatitis, vitiligo, pyoderma gangrenosum), confirming the therapeutic efficacy of the method without significant adverse effects. For the first time, low-temperature atmospheric plasma is considered in the context of skin microbiome modulation, introducing the concept of using this method not only for the elimination of pathogens but also for the restoration of microbial balance. A fundamentally novel aspect is the analysis of low-temperature atmospheric plasma for transdermal drug delivery through the effect of transient changes in cell membrane permeability.
The review also highlights current limitations in standardizing plasma treatment parameters and underscores the need for large-scale randomized studies with the aim to develop personalized treatment protocols. This work provides a theoretical foundation for further research into low-temperature atmospheric plasma as a promising alternative to traditional therapeutic methods in dermatology.
 449-459
449-459


Filaggrin: a key to understanding and treating atopic dermatitis
Abstract
Atopic dermatitis is a chronic inflammatory genetically determined skin disease characterized by high prevalence and a significant negative impact on patients’ quality of life. Impairment of the skin barrier in atopic dermatitis is closely associated with filaggrin deficiency—a key structural protein of the epidermis. Loss-of-function mutations in the FLG gene are a major genetic risk factor for atopic dermatitis, significantly worsening its course and prognosis.
Currently, active research is underway to develop effective methods for restoring filaggrin deficiency, which represents a promising approach in the therapy of atopic dermatitis. This article provides a systematic scientific data analysis in the PubMed, Google Scholar, and ClinicalTrials.gov databases to identify modern approaches to restoring the skin barrier in atopic dermatitis by targeting filaggrin and its metabolism. The following promising strategies for targeting filaggrin have been identified: direct replacement therapy with recombinant forms of filaggrin, the use of metabolites (L-histidine, cis-urocanic acid), plant extracts, and mechanical stimulation methods. These approaches demonstrate the potential to improve skin barrier function and reduce inflammation; however, further studies are needed to confirm their clinical efficacy and clarify mechanisms of action.
Modern strategies for correcting filaggrin deficiency hold significant therapeutic potential for atopic dermatitis but require further research, including at the molecular and clinical levels, to enable their integration into clinical practice.
 460-469
460-469


Isotretinoin Lidose in clinical practice
Abstract
Background: Systemic isotretinoin is recommended for the treatment of moderate to severe acne. The specialized Lidose modified-release technology has improved isotretinoin absorption in the gastrointestinal tract, increasing its bioavailability by 20%, thereby allowing a 20% dose reduction without compromising therapeutic efficacy.
Aim: The work aimed to estimate the clinical outcomes of isotretinoin Lidose in the treatment of moderate to severe acne.
Methods: A retrospective, uncontrolled, single-center study analyzed 2477 cases of systemic isotretinoin prescription in patients with moderate to severe acne, including 1912 women (77.2%) and 565 men (22.8%), with a mean age of 22.7 years; 290 patients (11.7%) had comorbidities. The daily therapeutic dose was calculated based on 0.4–0.8 mg/kg body weight, with a cumulative dose of 100–150 mg/kg. All patients underwent laboratory testing (complete blood count and biochemistry) before treatment, at 3 months, and at the end of therapy. For one month before systemic isotretinoin treatment, throughout the entire treatment course, and for one month after completion, female patients were advised to use at least one (preferably two) effective contraceptive method, including barrier contraception.
Results: After 6–12 months, all patients achieved complete clinical remission. By the end of therapy, skin oiliness and comedones disappeared, inflammatory lesions completely resolved, and skin texture became even. Among adverse events, cheilitis and xerosis were most frequently observed by weeks 2–3 and were successfully managed with moisturizers and lip balms. Transient elevations in transaminases and total cholesterol (within 10% of the normal range) were observed in 3.4% of cases, not requiring dose adjustment.
Conclusion: Systemic isotretinoin administration for moderate to severe acne allows achieving long-term clinical remission, which leads to a positive effect in preventing acne-related emotional distress. Retrospective analysis of isotretinoin Lidose use in clinical practice confirms not only its good tolerability but also its high efficacy in the treatment of moderate to severe acne.
 470-476
470-476


Autoimmune pemphigus: diagnostic challenges, interdisciplinary interaction, and therapeutic errors
Abstract
Patient safety is a fundamental principle in the provision of medical care. In the Russian Federation, continuous efforts are undertaken to reduce the number of adverse events, including through systematic analysis of medical errors and undesirable incidents. To illustrate these issues, the article presents four clinical cases of patients with various forms of acantholytic pemphigus. Particular attention is given to the young age of the patients and the clinical course of specific forms of acantholytic pemphigus. The paper discusses shortcomings in medical care, including violations of differential diagnostic algorithms, lack of interdisciplinary continuity, and therapeutic strategy failures. It is reported that diagnostic and therapeutic errors contribute to a more severe course of dermatosis and the transformation of one pemphigus form into another.
Timely diagnosis of pemphigus, which belongs to the group of autoimmune bullous dermatoses, is a crucial step in patient management and prevents progression of autoimmune forms in the absence of pathogenetic therapy. Diagnostic criteria include medical history, clinical presentation, cytological examination for acantholytic cells from the base of mucosal and/or skin erosions, histopathological examination of skin biopsy samples from lesions (including direct immunofluorescence methods), and/or indirect immunofluorescence testing of serum to detect IgG and IgA autoantibodies.
The article emphasizes the importance of adherence to clinical guidelines, increasing awareness among physicians of related specialties about current features of bullous dermatoses, and improving coordination among specialists from different disciplines. Addressing these issues will improve the quality of medical care and enhance patient safety.
 477-488
477-488


Circadian rhythms and atopic dermatitis
Abstract
The circadian rhythm is a 24-hour periodic cycle determined by the Earth’s rotation that modulates the behavior, physiology, and metabolism of all living organisms on our planet. The system that controls the circadian rhythm is known as the circadian clock. The mechanism of the circadian clock plays a crucial role in organismal development and functioning. For a long time, circadian clocks operated normally, being dependent on the alternation of light and darkness; however, lifestyle changes (artificial lighting, electronic devices, mobile phones, television, long-distance flights, etc.) have profoundly affected circadian rhythms. The resulting disruptions have led to health problems considered significant in the development of a number of diseases (malignant tumors, cardiovascular diseases, metabolic disorders, obesity, immune dysfunction).
In the skin, circadian rhythms are reflected in daily changes in transepidermal water loss, permeability and microcirculatory function, pruritus intensity, sleep–wake cycle, and the activity of the innate and adaptive immune systems. At the cellular level, the circadian rhythm regulates the mitotic cell cycle, keratinocyte differentiation timing, and many other processes. In atopic dermatitis, a vicious cycle exists: pruritus worsens sleep quality, leading to chronic stress, thereby disrupting the sleep–wake circadian rhythm; in turn, sleep deprivation, poor sleep quality, and chronic stress aggravate pruritus. These processes trigger exacerbations of atopic dermatitis, in which both pruritus and poor sleep quality intensify, significantly impairing the rhythmic functioning of the whole body and the skin in particular.
Recognizing the importance of circadian skin functions and the consequences of their disruption allows physicians to optimize therapy and maximize efficacy of prescribed treatment. Many topical agents may provide greater benefit if circadian rhythms are taken into account, whereas lower doses or less potent formulations could be sufficient.
 489-497
489-497


Therapeutic potential of prostaglandins in dermatology: focus on vitiligo
Abstract
This article presents an analysis of the therapeutic potential of prostaglandins in dermatology, with an emphasis on their application in vitiligo.
Prostaglandins are a group of low-molecular-weight lipid eicosanoids capable of regulating numerous physiological processes, including renal function, platelet aggregation, neurotransmitter release, and immune system activity, as well as influencing the skin, gastrointestinal tract, and reproductive system. The ubiquitous presence of prostaglandins in body tissues and their involvement in the regulation of inflammatory, regenerative, and proliferative processes make these molecules a promising subject for dermatological research.
The therapeutic potential of prostaglandins in dermatology extends far beyond their initial indications. Due to their unique properties, prostaglandins exert a complex effect: on the one hand, they activate melanocytes and stimulate melanogenesis; on the other hand, they modulate immune responses by suppressing autoimmune reactions. This article provides a detailed examination of the mechanisms of action of prostaglandins, including their role in inflammation regulation and their interaction with receptors in the skin. The advantages of prostaglandins in combination therapy for vitiligo are discussed, particularly in conjunction with phototherapy, microneedling, and laser-based methods. The article presents data demonstrating the high efficacy of prostaglandins in treating vitiligo, especially in resistant forms of the disease. The authors emphasize that prostaglandin-based therapy may significantly enhance vitiligo treatment outcomes by increasing repigmentation stability and providing more sustained results. The article also highlights the need for further research to optimize dosing regimens, treatment protocols, and duration of prostaglandin therapy.
This review article is based on a systematic search of scientific data (original research, clinical studies, reviews, and guidelines) reflecting current insights into the role of prostaglandins in dermatology and their therapeutic potential in vitiligo over 1987 to 2025 from PubMed, Scopus, Web of Science, and eLibrary.ru.
 498-506
498-506


CHRONICLES
Chronicles of A.I. Pospelov Moscow Society of Dermatovenerologists and Cosmetologists (MSDС founded on October 4, 1891). Bulletin of the MSDС No. 1161
Abstract
The 1161st meeting of the A.I. Pospelov Moscow Society of Dermatovenerologists and Cosmetologists was held on February 18, 2025.
The meeting, which included both clinical and scientific sections, took place in person in the conference hall of the V.A. Rakhmanov Clinic of Skin and Venereal Diseases (Sechenov University). A total of 110 participants attended. Nine membership applications were submitted to the Society—all from residents and staff members of the Department of Dermatovenereology at the N.I. Pirogov Russian National Research Medical University.
The clinical section featured a presentation on sarcoidosis with two patient cases, which expanded the general understanding of specific and nonspecific skin lesions. Another case report on subcorneal pustular dermatosis (Sneddon–Wilkinson disease) highlighted the subtleties of differential diagnosis with pustular psoriasis, impetigo, herpes gestationis, acantholytic pemphigus, and other conditions. It was emphasized that clinical presentation and histological examination are decisive in diagnosing this rare, chronic, benign, relapsing neutrophilic pustular dermatosis.
The scientific section opened with a report on Alexey I. Pospelov—the founder of the Moscow Scientific Society of Dermatologists and Venereologists and one of the key figures in the development of the Russian dermatological school. Professor Pospelov described oral mucosal involvement in lichen planus and psoriasis, idiopathic skin atrophy, advocated for the use of X-rays in diagnosing syphilitic bone lesions, and predicted their potential for therapeutic use, but also cautioned against adverse effects. He also developed the neurogenic theory of skin diseases and of alopecia areata.
Two additional reports in the scientific section addressed clinical manifestations of onychodystrophies and dermatoses associated with diabetes mellitus.
 507-512
507-512


PHOTO GALLERY
Herpes zoster: a photo gallery
Abstract
Herpes zoster is a viral disease. Its development is directly related to the reactivation of the human herpesvirus type 3. At certain points in life, 10%–20% of the population is at risk of developing this condition. The likelihood of disease increases significantly in immunocompromised individuals, including those with HIV infection, malignancies, or those who have undergone bone marrow transplantation, or are receiving long-term cytostatic or systemic glucocorticoid therapy. In people living with HIV, herpes zoster occurs 8–15 times more frequently than in the general population. In immunodeficient states, including HIV-associated immunodeficiency, the course of herpes may have distinct features.
This photo gallery presents cases of herpes zoster that developed in the setting of HIV infection. In such cases, clinical manifestation typically occurs when CD4+ T-cell counts fall below 400 cells/μL. In patients not receiving antiretroviral therapy, deeper immunosuppression may lead to recurrence. In some patients with low immune status, herpes zoster may appear as a manifestation of immune system reconstitution inflammatory syndrome. The severity and clinical presentation of the disease are largely determined by the degree of immunodeficiency. In HIV-infected individuals, multidermatomal involvement—affecting two or more dermatomes simultaneously—is common. Compared to HIV-negative individuals, the vesicular eruption phase may last more than 10 days, and atypical forms are more frequently observed (e.g., hemorrhagic, ulceronecrotic, verrucous, disseminated, generalized), which may occur in combination and present with more intense and deeper skin lesions. In HIV-infected individuals, localization of lesions in the external auditory canal is associated with a high risk of auditory involvement, whereas localization in the area innervated by the ophthalmic branch of the trigeminal nerve implies a risk of visual impairment. One possible complication is Ramsay Hunt syndrome (characterized by vesicles in the auricular region, ear pain, and facial nerve paresis or paralysis).
According to the Russian clinical classification, the first episode of herpes zoster in a person living with HIV may serve as the basis for diagnosing stage 2B (acute HIV infection with secondary diseases) or stage 4A (secondary diseases) depending on the duration of HIV infection. Recurrent or disseminated herpes zoster corresponds to stage 4B.
This photo gallery presents various clinical forms and anatomical locations of herpes zoster in patients with HIV infection. The descriptions of the lesions specify their location in accordance with the innervation zones of peripheral sensory nerves.
All photographs presented in this article are from the author’s personal archive.
 513-520
513-520