Том 24, № 2 (2021)
- Год: 2021
- Выпуск опубликован: 15.04.2021
- Статей: 11
- URL: https://rjsvd.com/1560-9588/issue/view/3841
- DOI: https://doi.org/10.17816/dv.242
Весь выпуск
ДЕРМАТООНКОЛОГИЯ
Физиологические функции рецепторов эпидермального фактора роста кератиноцитов и их роль в развитии нежелательных реакций в процессе таргетной терапии злокачественных новообразований
Аннотация
Связывание рецепторов эпидермального фактора роста (EGFR) является хорошей мишенью для лечения рака лёгких, толстой кишки, поджелудочной железы, головы и шеи. Развивающиеся в результате терапии нежелательные явления в виде поражения кожных покровов и слизистых оболочек представляют серьёзную проблему для выбора врачом долгосрочной тактики лечения. Симптомы кожной токсичности, как часто называют проблемы с кожей у пациентов, вызывают беспокойство и часто влияют на качество жизни и соблюдение режима лечения. Таким образом, для врачей важно знать предпосылки и способы управления кожной токсичностью, связанной с использованием ингибиторов тирозинкиназного рецептора эпидермального фактора роста.
Описан механизм и последствия активации рецепторов EGF, объясняющие развитие нежелательной кожной токсичности, связанной с ингибированием EGFR.
 111-118
111-118


ДЕРМАТОЛОГИЯ
Фармакогенетический подход к прогнозированию безопасности терапии метотрексатом у больных псориазом
Аннотация
Метотрексат является высокоэффективным средством терапии среднетяжёлых и тяжёлых форм псориаза, однако его токсичность у некоторых пациентов ограничивает его применение. У 10–30% пациентов токсическое действие метотрексата приводит к необходимости отмены препарата. Установлено, что генетические факторы играют существенную роль в индивидуальном ответе пациентов на терапию. Выявлены и активно изучаются аллельные варианты различных генов, носительство которых предрасполагает к развитию нежелательных лекарственных реакций при терапии метотрексатом. Фармакогенетические исследования позволяют установить, каким образом генотип пациента оказывает влияние на безопасность лечения метотрексатом. По данным современных исследований, для прогнозирования риска метотрексатиндуцированной токсичности необходимо учитывать индивидуальные особенности его фармакокинетики, которые определяются наличием однонуклеотидных полиморфизмов генов, кодирующих белки-переносчики метотрексата и ферменты его биотрансформации. Активность белков-транспортёров оказывает влияние на концентрации препаратов в плазме крови и периферических тканях, тем самым определяя его токсичность.
В данной статье мы рассматриваем изученные на сегодняшний день генетические полиморфизмы, определяющие вариабельность токсичности метотрексата.
Применение фармакогенетического подхода к прогнозированию риска развития нежелательных лекарственных реакций метотрексата поможет персонализировать терапию пациентов с псориазом.
 119-132
119-132


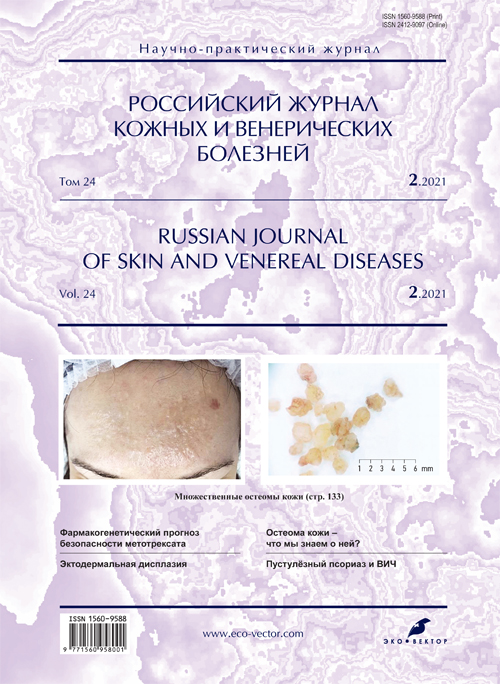
Что мы знаем об остеоме кожи? Обзор литературы. Клинические случаи
Аннотация
В статье обобщены данные по эпидемиологии, этиопатогенезу, клинической картине, диагностике и лечению остеомы кожи. Представлены классификация, гистологическая картина, место остеомы кожи с точки зрения фенотипа согласно сведениям мировой литературы.
Остеома кожи является редким доброкачественным заболеванием, характеризующимся образованием костной ткани в дерме или подкожно-жировой клетчатке. Особый интерес представляют две теории возникновения остеомы кожи ― результат метаплазии фибробластов в остеобласты либо дифференцировка примитивных мезенхимальных клеток в остеобласты и их миграция в эктопическое место. Диагностика и дифференциальный диагноз основываются на клиническом обследовании, измерении уровня кальция, паратиреоидного гормона, рентгенологических методах и биопсии кожи. В дифференциальный диагноз входит множество дерматозов, включая оссифицированный волосяной фолликул, остеосаркому, эпидермоидные кисты, фибромы, нейрофибромы, базальноклеточный рак и т.д. Подход к лечению заключается в применении неинвазивных или инвазивных методов: крем третиноин, дермабразия и панч-биопсия, YAG-лазер, иссечение скальпелем, кюретаж и СО2-лазер.
Мы считаем остеому кожи недооценённым дерматозом, поскольку в доступной нам отечественной литературе мы не встретили описания подобных случаев и литературных обзоров.
 133-144
133-144


Подострая диссеминированная микробная экзема у подростка
Аннотация
Микробная экзема среди различных клинических форм экзем в структуре заболеваемости занимает второе место после истинной. Чаще болеют взрослые, дети ― крайне редко. В основе патогенеза микробной экземы лежат нарушения иммунного статуса и микробная сенсибилизация организма, что обусловлено фоновыми очагами инфекции, а также дисбиозом в микробиоме организма. Для клинической картины болезни характерна асимметричная локализация высыпаний на конечностях в виде единичных бляшек. Поражённая кожа красноватая, сквамозная, слабо инфильтрирована. Вне основных очагов наблюдаются папуловезикулёзные и пустулёзные элементы, корки. Высыпания не всегда сопровождаются зудом. Микробная экзема ограниченного характера проявляется монетовидными очагами, точечным мокнутием, корками.
Под нашим наблюдением находилась пациентка в возрасте 15 лет, которая до поступления в стационар болела уже 8 месяцев, при этом в течение 3 последних месяцев патологический процесс на коже протекал остро, без какой-либо динамики. Возникновение высыпаний ни с чем не связывала. Множественные эффлоресценции располагались по всему кожному покрову, на волосистой коже головы, ушных раковинах, в заушной области, на лице, шее, туловище, верхних и нижних конечностях, ягодицах; сопровождались сильным зудом. Островоспалительный патологический процесс был представлен экскориациями, мокнущими пятнами, эрозиями, корками и эритематозно-сквамозными очагами различных очертаний и размеров. Дермографизм розовый. Неоднократное амбулаторное лечение приносило временное улучшение. Из-за отсутствия лечебного эффекта в последние 3 месяца больная была госпитализирована в стационар филиала «Коломенский». При комплексном клинико-лабораторном обследовании был поставлен диагноз диссеминированной подострой микробной экземы.
На фоне адекватной терапии островоспалительный патологический процесс полностью разрешился. Пациентке даны рекомендации для поддержания достигнутого лечебного эффекта.
Описанный случай представляет интерес своей относительной редкостью в детской популяции.
 145-150
145-150


Пустулёзный псориаз и артропатия у больного ВИЧ-инфекцией. Клинический случай
Аннотация
В статье представлен клинический случай сочетания нескольких форм псориаза (вульгарного, пустулёзного) и артропатии у больной ВИЧ-инфекцией. Диагноз псориаза подтверждён морфологическим исследованием. Признаки артропатии установлены при рентгенографии: выявлено наличие олигоартрита дистальных межфаланговых суставов пальцев кистей и стоп. Степень выраженности дактилита ― 2–3 балла, индекс Ричи ― 2, дерматологический индекс качества жизни ― 28. Обсуждается необходимость междисциплинарного подхода к лечению данной больной с учётом коморбидного состояния. Рассматриваются варианты клинического течения псориаза и особенности его лечения у ВИЧ-инфицированных больных с учётом данных литературы и собственного наблюдения. Представленный случай является иллюстрацией особенностей течения и коморбидности хронического дерматоза и СПИДа, обусловленного влиянием инфекционного процесса, иммуносупрессии и антиретровирусной терапии. Развитие пустулёзной формы и артропатии создаёт дополнительную проблему назначения базового системного лечения при тяжёлом и осложнённом псориазе у ВИЧ-инфицированного больного из-за наличия противопоказаний, обусловленных коморбидностью. Комиссионно выбранный глюкокортикостероид оказался эффективным в отношении кожного и суставного процесса, не оказав негативного воздействия на течение и терапию ВИЧ-инфекции. Терапевтические методики для категории пациентов с коморбидностью требуют дальнейших разработок с последующим их включением в дополнительный раздел клинических рекомендаций по диагностике и лечению псориаза.
 151-160
151-160


Способы камуфляжа витилиго (обзор литературы)
Аннотация
Витилиго значительно влияет на качество жизни пациентов, их социальную и психологическую адаптацию в обществе. Отмечено, что у пациентов с витилиго чаще развиваются тревожные и депрессивные расстройства, суицидальные мысли. Стандартные схемы терапии на сегодняшний день зачастую занимают продолжительное время, недостаточно эффективны и не всегда соответствуют ожиданиям пациента и врача-дерматовенеролога, что снижает приверженность к лечению. В связи с этим комплексная терапия витилиго до сегодняшнего дня остаётся актуальным вопросом.
Медицинский камуфляж является перспективным методом дополнительной или альтернативной терапии витилиго, так как позволяет контролировать клинические проявления заболевания.
Задачей данного обзора было изучение основных видов медицинского камуфляжа на российском и зарубежном рынках, их доступность и принцип действия. Проанализирована литература с использованием базы данных PubMed, а также сети Интернет по теме использования медицинского камуфляжа пациентами с витилиго с целью выявить наиболее эффективные, доступные и простые в использовании продукты, которые можно приобрести на российском и зарубежном рынках. В ходе анализа определены наиболее значимые средства, максимально удобные в нанесении на кожу и легкодоступные для приобретения больными витилиго в России. Оценивались такие параметры, как форма, текстура, состав и длительность эффекта. Подробно описана каждая группа препаратов, а также техника их правильного применения.
Данный обзор обращён к практикующим дерматовенерологам, заинтересованным в вопросах контроля течения и клинических проявлений витилиго.
 161-166
161-166


Системная терапия онихомикозов стоп тербинафином: динамика санации ногтей и качества жизни (многоцентровое наблюдательное исследование)
Аннотация
Обоснование. Системная терапия тербинафином (Экзифин®) составляет основу любых программ лечения онихомикозов стоп дерматомицетной этиологии. Вместе с тем в доступной литературе представлено относительно мало данных по эффективности и безопасности системных препаратов тербинафина по отдельным возрастным группам и практически отсутствуют такие работы на основе большой статистической выборки с одновременной оценкой динамики показателя качества жизни.
Цель ― изучить применение лекарственного препарата Экзифин® (таблетки) в отдельных возрастных группах пациентов с микозом и онихомикозом в клинической практике.
Материал и методы. Выполнено многоцентровое наблюдательное (неинтервенционное) исследование, в котором приняли участие 1602 пациента с различной степенью тяжести онихомикоза стоп/кистей. Пациенты были распределены на 4 возрастные группы, в каждой из которых выделялись подгруппы по тяжести течения онихомикоза ― от очень лёгкого до чрезвычайно тяжёлого. Оценивались положительная динамика регресса симптомов, улучшение качества жизни по опросной шкале, наличие или отсутствие существенных нежелательных реакций.
Результаты. У всех пациентов получена положительная динамика со стороны кожного процесса в виде регресса симптомов онихомикоза. Наилучшие результаты по скорости санации ногтей отмечены в более молодых возрастных группах с лёгкой степенью онихомикоза. Наименьшая скорость отрастания здоровой ногтевой пластинки отмечена в возрастных группах 45–60 и старше 60 лет. В этих же возрастных группах отмечено наибольшее количество стойких ониходистрофий, даже после эрадикации гриба. Во всех возрастных группах имела место положительная динамика качества жизни: в конце лечения качество жизни 67% пациентов оценивали как «прекрасно» и «хорошо», ещё 24,1% ― как «удовлетворительно». Ни в одном клиническом случае не было зафиксировано нежелательных явлений.
Заключение. Системная терапия тербинафином при онихомикозе стоп/кистей является высокоэффективным компонентом в составе комбинированного лечения, позволяющим достигать эрадикации гриба в 85–90% случаев.
 167-178
167-178


Клинический опыт наблюдения и тактика ведения пациента с эктодермальной ангидротической дисплазией
Аннотация
Понятие «эктодермальные дисплазии» охватывает группу редких наследственных аномалий развития, имеющих многообразие фенотипических вариантов, но характеризующихся общими признаками недоразвития или аномалийного формирования органов и тканей, производных эктодермального листка (кожа и её дериваты ― ногти, волосы, зубы, нервная система и органы чувств). Примерно 25% известных до настоящего времени эктодермальных дисплазий наследуются по аутосомно-доминантному или аутосомно-рецессивному типу, в остальных случаях тип наследования невыяснен. Синдром характеризуется широким спектром клинических проявлений и может включать дополнительные симптомы поражения других эктодермальных, мезодермальных и эндодермальных структур. Эктодермальные аномалии ― проявление нарушений в пространственно-временной координации в ходе развития эпидермиса. В них участвуют такие гены, как EGF (эпидермальный фактор роста), ЕD1 (эктодисплазин), EDAR (ангидротический рецептор эктодисплазина 1) и другие, активирующие или подавляющие факторы транскрипции (в частности рбЗ; Koster). Выявлено пока лишь около 20% генов, отвечающих примерно за 200 эктодермальных дисплазий различной симптоматики и степени выраженности.
В статье описывается клиническое наблюдение пациента с редким заболеванием ― эктодермальной ангидротической дисплазией. Представленны данные литературы о клинических особенностях течения дерматоза, в том числе у описываемого нами пациента.
 179-186
179-186


КОСМЕТОЛОГИЯ
Оценка эффективности и безопасности фотодинамической терапии кожи
Аннотация
Обоснование. Фотодинамическая терапия ― инновационная методика неинвазивного омоложения кожи за счёт стимуляции неоколлагеногенеза.
Цель ― оценка безопасности и эффективности воздействия на кожу фотодинамической терапии мощностью 660 нм с использованием геля Сферометаллохлорин™ в качестве фотосенсибилизатора.
Материал и методы. Выполнено нерандомизированное контролируемое клиническое исследование. Первый этап исследования, в котором участвовали 5 лабораторных крыс женского пола, был разделён на 2 подэтапа: 1А ― воздействие источником облучения длиной волны 660 нм (энергия 100 Дж/см2, мощность 100 мВ/см2) на слизистую оболочку полости рта в течение 30 мин; 1Б ― дополнительное использование геля, содержащего 0,4% Сферометаллохлорин™, в качестве фотосенсибилизатора, при тех же условиях облучения.
Второй этап исследования с участием 15 женщин-добровольцев в возрасте от 21 до 65 лет также был разделён на два подэтапа: 2А ― облучение заушной области в течение 30 мин длиной волны 660 нм (энергия 100 Дж/см2, мощность 100 мВ/см2) с использованием в качестве фотосенсибилизатора 0,4% геля, содержащего Сферометаллохлорин™, 2Б ― оценка эффективности воздействия курса процедур фотодинамической терапии на кожу при помощи кутометрии, корнеометрии, измерения трансэпидермальной потери воды.
Во всех случаях оценку безопасности проводили с помощью гистологического исследования (панч-биопсия). Кроме того, проводили фотографирование и оценку нежелательных эффектов.
Результаты. По данным гистологического исследования, воздействие излучением 660 нм на слизистую оболочку полости рта крысы не вызывает каких-либо отклонений от нормы; при воздействии излучением 660 нм с использованием фотосенсибилизатора на кожу заушной области женщин появляются небольшая отёчность и набухание ядер эпидермиса, которые полностью разрешаются через 20 дней. Используемое излучение длиной волны 660 нм является полностью безопасным, не вызывает патологических изменений в коже. Используемый в качестве фотосенсибилизатора гель, содержащий 0,4% Сферометаллохлорин™, хорошо проникает в дерму, оптимальное время экспозиции составляет 30 мин. Курс процедур фотодинамической терапии является безопасным, эффективным методом, вызывающим ремоделирование дермы.
Заключение. Фотодинамическую терапию с использованием излучения 660 нм и Сферометаллохлорина™ в качестве фотосенсибилизатора можно рекомендовать для использования в практическом здравоохранении.
 187-196
187-196


ХРОНИКА
Хроника Московского общества дерматовенерологов и косметологов имени А.И. Поспелова (МОДВ основано 4 октября 1891 г.)Бюллетень заседания МОДВ № 1141
Аннотация
19 января 2021 года состоялось очередное, 1141-е заседание Московского общества дерматовенерологов и косметологов имени А.И. Поспелова. В повестке дня были следующие вопросы: прием в члены МОДВ, разбор 3 клинических случаев, заслушивание научных докладов.
 197-200
197-200


ФОТОГАЛЕРЕЯ
Фотогалерея. Саркоидоз (часть 1)
Аннотация
Саркоидоз (син.: болезнь Бенье–Бека–Шауманна, доброкачественный гранулематоз, хронический эпителиоидно-клеточный ретикулоэндотелиоз) ― мультисистемное заболевание из группы гранулематозов неизвестной этиологии, морфологической особенностью которого является развитие эпителиоидно-клеточных гранулём без казеозного некроза с процессами дистрофии, деструкции и фиброзирования в тканях различных органов. С учётом разнообразия клинических поражений выделяют три основные формы ― внегрудную, внутригрудную, смешанную (генерализованную).
 201-206
201-206