Intravascular histiocytosis of the skin
- Authors: Bulanov D.V.1, Podverbnaya J.S.1
-
Affiliations:
- The Russian National Research Medical University named after N.I. Pirogov
- Issue: Vol 28, No 3 (2025)
- Pages: 293-300
- Section: DERMATOLOGY
- Submitted: 09.02.2025
- Accepted: 02.06.2025
- Published: 27.07.2025
- URL: https://rjsvd.com/1560-9588/article/view/653977
- DOI: https://doi.org/10.17816/dv653977
- EDN: https://elibrary.ru/TGCNMF
- ID: 653977
Cite item
Abstract
Intravascular histiocytosis is a rare dermatologic condition characterized by pathological vascular dilation and accumulation of histiocytes within the lumen of blood vessels. Despite its rarity, challenges in diagnosis and treatment persist due to the absence of standardized protocols and a limited understanding of the disease pathogenesis.
A key initiating factor is damage to the vascular wall, promoting histiocyte migration and proliferation within vessels. This process may be triggered by infections, cardiovascular dysfunction, hepatic or renal pathology. However, some cases occur in individuals without comorbidities, suggesting the involvement of unidentified triggers or genetic predispositions.
Clinical manifestations vary and include ill-defined erythematous to violaceous patches, plaques, nodules, and papules, most commonly affecting the trunk and extremities. The lesions may also present as hemorrhagic nodules and papules, complicating the differential diagnosis with other dermatoses. The condition’s rarity and non-specific presentation often result in misdiagnosis and inappropriate treatment, worsening the clinical course.
Currently, there is no universal treatment protocol for intravascular histiocytosis. Corticosteroids are frequently used, but their efficacy and long-term outcomes remain poorly defined.
This article describes a clinical case of a female patient presenting with papular eruptions on the neck and scalp. The diagnosis was confirmed by dermatoscopy and histological examination of a skin biopsy. The case highlights the need for further research to establish standardized diagnostic and therapeutic strategies for intravascular histiocytosis.
Keywords
Full Text
АКТУАЛЬНОСТЬ
Внутрисосудистый гистиоцитоз, также известный как интраваскулярный гистиоцитоз, представляет собой редкое дерматологическое заболевание, которое характеризуется аномальным расширением сосудистого просвета с накоплением в нём гистиоцитов ― клеток иммунной системы, участвующих в процессах фагоцитоза и воспалительного ответа [1]. Это состояние привлекает внимание учёных своей редкостью и сложностью диагностики. Впервые термин «внутрисосудистый гистиоцитоз» был предложен в 1994 году J.T. O’Grady [2], который подробно описал клиническую картину заболевания. С тех пор патология была включена в более широкую категорию внутрилимфатического гистиоцитоза. Дальнейшие исследования позволили выделить два различных типа доброкачественных новообразований, различающихся механизмом образования скоплений гистиоцитов внутри сосудов.
Особенность заболевания заключается в том, что подобные изменения могут быть обнаружены как в лимфатических, так и в кровеносных сосудах, что свидетельствует о системном характере процесса [3, 4]. Внутрисосудистый гистиоцитоз часто ассоциируется с ревматоидным артритом, предполагая возможную взаимосвязь между этими патологиями. У пациентов с ревматоидным артритом гистиоцитарные скопления наблюдаются преимущественно в лимфатических сосудах, что, возможно, указывает на общий патогенетический механизм. В отдельных случаях развитие гистиоцитарных скоплений затрагивает также кровеносные сосуды, что подчёркивает важность междисциплинарного подхода к диагностике и лечению данной патологии [5]. Согласно данным гистологического анализа, проведённого I. Catalina-Fernández и соавт. [5], внутрисосудистый гистиоцитоз представляет собой сложный многофакторный процесс. Биопсийные исследования продемонстрировали, что при определённых условиях патологический процесс может переходить за пределы лимфатической системы, поражая кровеносные сосуды и вызывая значительные изменения в сосудистой стенке. Это открытие подчёркивает важность тщательного изучения иммунных и воспалительных механизмов, лежащих в основе данного заболевания.
Внутрисосудистый гистиоцитоз: эпидемиология, этиология, патогенез
Эпидемиологические исследования показывают, что внутрисосудистый гистиоцитоз встречается преимущественно у женщин. Заболевание чаще всего развивается у взрослых и пожилых пациентов, что, возможно, связано с возрастными изменениями в иммунной системе и сосудистой ткани, однако точные причины гендерной предрасположенности и возрастного распределения остаются невыясненными и требуют дальнейших исследований. Таким образом, внутрисосудистый гистиоцитоз представляет собой редкое и сложное заболевание, требующее глубокого междисциплинарного подхода к его изучению.
Патогенез и этиология внутрисосудистого гистиоцитоза остаются предметом активного научного изучения, поскольку данные о механизмах его возникновения и развития всё ещё ограничены. За время исследований взгляды на этиопатогенез претерпели значительные изменения, отражая постепенное накопление новых знаний о природе заболевания. На начальных этапах изучения внутрисосудистого гистиоцитоза основное внимание уделялось внешним факторам, которые могли быть связаны с развитием заболевания. В качестве ключевых факторов риска рассматривались воздействие рентгеновского излучения, контакт с химическими растворителями, гемотрансфузии в детском возрасте, а также перенесённые инфекционные заболевания в неонатальном и раннем детском периодах [6, 7]. Эти гипотезы базировались на наблюдениях, связанных с воздействием факторов окружающей среды и их предполагаемым влиянием на иммунную систему. Одной из ранних гипотез, активно обсуждавшихся в научной литературе, была инфекционная природа внутрисосудистого гистиоцитоза. Учёные выдвигали предположение, что иммунная система человека имеет способность реагировать на вторжение чужеродного микроорганизма изменениями воспалительного характера, свойственными для данного заболевания, тем не менее присутствия бактериальных или вирусных микроорганизмов в поражённых тканях в ходе различных лабораторно-инструментальных исследований не обнаружено, что и привело к отказу от данной гипотезы [8].
На данный момент времени установлено, что внутрисосудистый гистиоцитоз имеет неопластическое происхождение и относится к группе так называемых случайных пролиферативных процессов, при которых стартовые мутации, определяющие формирование опухолевого клона, происходят спонтанно. Достижение этого понимания стало возможным благодаря прогрессу в области молекулярной генетики. Исследования показали, что клетки, обнаруживаемые в поражённых тканях при внутрисосудистом гистиоцитозе, имеют клональное происхождение и относятся к миелоидному ряду [9, 10]. Особое внимание было уделено мутациям онкогена BRAF, в частности мутации BRAF-V600E, которая выявляется более чем в 50% случаев внутрисосудистого гистиоцитоза. Впервые эту мутацию описали G. Badalian-Very и соавт. [11], а позднее её высокая частота была подтверждена в независимых исследованиях на различных когортах пациентов [11–13]. Эти открытия позволили глубже понять молекулярные механизмы заболевания и создать основу для разработки потенциальных таргетных терапий.
Несмотря на успехи молекулярной биологии, в научном сообществе продолжают обсуждаться различные теории патогенеза внутрисосудистого гистиоцитоза. Одной из гипотез является нарушение целостности сосудистой стенки, что создаёт условия для миграции и пролиферации гистиоцитов. Согласно исследованиям E. Rieger и соавт. [3], тромботическая окклюзия мелких сосудов может приводить к проникновению в кровоток различных веществ, таких как криоглобулины, которые инициируют репаративные и воспалительные процессы. Эти процессы включают активацию фагоцитарной системы и запускают пролиферацию гистиоцитов как одну из реакций. Роль воспаления также рассматривалась в контексте воздействия провоспалительных цитокинов. Например, фактор некроза опухоли альфа (tumor necrosis factor alpha, TNF-α) был выделен N. Okamoto и соавт. [14] как возможный медиатор воспалительного ответа, связанный с ревматоидным артритом. Однако взаимосвязь между внутрисосудистым гистиоцитозом и ревматоидным артритом остаётся дискуссионной, так как не всегда выявляется совместное присутствие этих патологий у одного пациента [15]. Инфекционные процессы также могут играть косвенную роль в патогенезе. Согласно предположению K. Asagoe и соавт. [4], бактериальные инфекции способны повреждать сосудистую стенку, вызывая активацию врождённого иммунитета и миелоидных клеток. Эта гипотеза основана на наблюдениях гиперреактивности иммунной системы при некоторых бактериальных инфекциях, но требует дальнейшего подтверждения.
Клинические проявления
Кожные изменения при внутрисосудистом гистиоцитозе представляют собой один из ключевых диагностических признаков заболевания. В большинстве случаев они проявляются фиолетовыми пятнами, локализованными преимущественно на туловище и конечностях [16]. При внутрисосудистом гистиоцитозе, ассоциированном с ревматоидным артритом, кожные поражения часто возникают в области суставов, поражённых основным заболеванием, и в их непосредственной близости [17, 18]. Характерные симптомы внутрисосудистого гистиоцитоза включают плохо очерченные эритематозные пятна, бляшки, узелки и папулы. В некоторых случаях кожные изменения могут приобретать сетчатую форму, напоминающую ливедо, что затрудняет их дифференциальную диагностику с другими васкулопатиями [19]. Интересной особенностью являются папулёзные элементы, располагающиеся вдоль сосудистого русла в линейном, волнообразном или ветвистом порядке, что указывает на прямую связь патологического процесса с сосудами, подчёркивая сосудистую природу поражений [20]. Ещё одним важным симптомом внутрисосудистого гистиоцитоза является отёчность в поражённых областях, которая может быть выраженной и сопровождаться изменением цвета кожи [21]. Болевой синдром при внутрисосудистом гистиоцитозе наблюдается не у всех пациентов: одни могут испытывать дискомфорт или даже интенсивные болевые ощущения в зоне поражения, тогда как другие не предъявляют жалоб на болезненность [21, 22].
Прогноз и факторы риска
Прогноз при внутрисосудистом гистиоцитозе варьирует и зависит от множества факторов, среди которых выделяют возраст начала заболевания, при этом более ранний дебют часто ассоциируется с неблагоприятным исходом. Это связано с тем, что в детском возрасте заболевание может иметь более агрессивное течение, поражая не только кожу, но и внутренние органы. Другими значимыми факторами являются тип заболевания, площадь поражения, а также степень вовлечённости висцеральных органов. У пациентов с генерализованной формой внутрисосудистого гистиоцитоза, включающей поражение лёгких, сердца, центральной нервной системы или эндокринных органов, прогноз ухудшается. Такие осложнения, как несахарный диабет, эндокринопатии, поражение костной ткани, а также зубов, существенно увеличивают риск неблагоприятного исхода [23]. Летальность при внутрисосудистом гистиоцитозе возрастает в случае прогрессирующего течения заболевания, когда патологический процесс становится неконтролируемым. Прогрессирование сопровождается увеличением площади поражения, усилением воспалительных реакций и развитием осложнений, которые могут включать тяжёлые системные нарушения.
ОПИСАНИЕ СЛУЧАЯ
О пациенте
Пациентка Ш., 18 лет, обратилась к дерматологу с жалобами на состояние кожи в области шеи и волосистой части головы.
Анамнез заболевания. В 2020 году впервые заметила высыпания в виде розоватых узелков размером 1–2 мм в диаметре каждый. Со временем эти узелки начали расплываться, обесцвечиваться, а белые пятна, образованные на их месте, увеличивались в размере, при этом никаких неприятных ощущений не возникало. Пациентку ничего не беспокоило, она не обращалась к врачам-специалистам, в том числе к дерматологу, и, как следствие, никакого лечения ранее не проводилось.
Анамнез жизни. Сопутствующих заболеваний нет, однако пациентка наблюдается у эндокринолога в связи с диффузными изменениями щитовидной железы. За 4 месяца было замечено уменьшение массы тела на 6 кг без каких-либо ограничений в рационе. Пациентка отрицает употребление табака, алкоголя и наркотических средств. Генетические особенности и результаты аллергологического анализа не отличаются от стандартных.
Результаты физикального, лабораторного и инструментального исследования
При осмотре (status localis) поражение на кожном покрове имеет ограниченный характер. Локализуется в только в верхней части тела пациента, а именно на передней, правой боковой, заднебоковой и задней поверхностях шеи. На передней и правой боковой поверхностях шеи в процессе осмотра обнаруживаются папулы, размер которых достигает 2–4 мм в диаметре (рис. 1). Папулы имеют беловатый оттенок, содержат в себе вкрапления розоватых точек в центральной части, имеют плотную консистенцию. Одна из папул расширилась до размеров бляшки, диаметр которой составил до 1,5 см. Поражение на заднебоковой поверхности шеи представлено геморрагическим узелком. Образование подобного рода, со слов пациентки, возникло около 2 месяцев назад. Геморрагический узелок увеличился в размерах с течением времени и стал более заметным. Субъективных ощущений нет. Кожа вне очагов представлена загаром серого цвета с чёткой нижней границей и более размытой верхней частью.
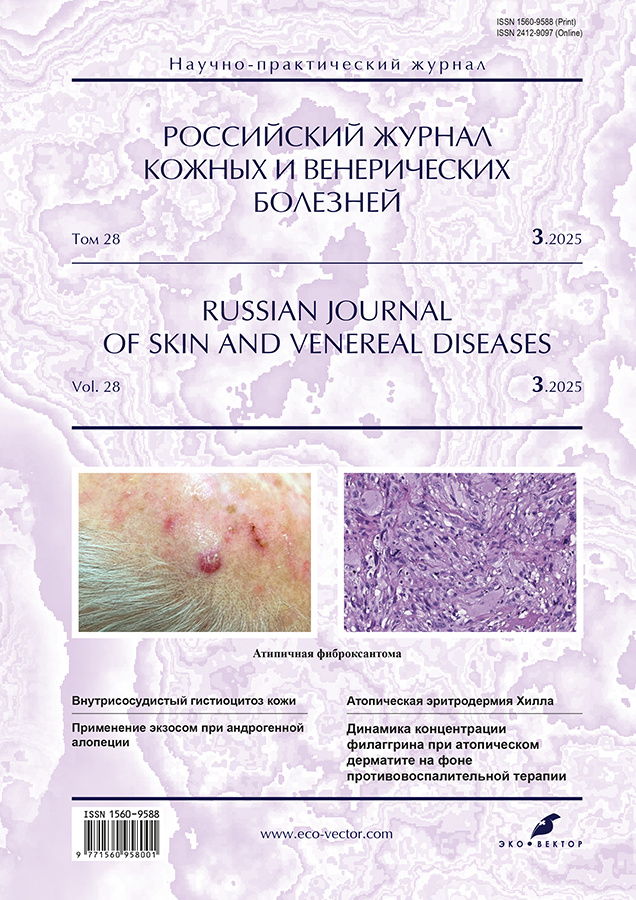
Рис. 1. Дерматоскопическая картина внутрисосудистого гистиоцитоза кожи: эритематозно-папулёзный элемент кожи передней поверхности шеи. [Фото из архива РНИМУ им. Н.И. Пирогова. Публикуется впервые с разрешения администрации учреждения].
Fig. 1. Dermatoscopic picture of intravascular skin histiocytosis: erythematous-papular element of the skin of the anterior surface of the neck. [Photo from the archive of the Russian National Research Medical University named after N.I. Pirogov. Published for the first time with the permission of the administration of the institution].
Лабораторно-инструментальная диагностика. Результаты проведённых исследований крови и мочи в пределах нормы. Результаты биохимического анализа крови свидетельствуют о некотором снижении уровня компонента C3 (73 мг/дл при норме 88–201). При гистологическом исследовании биоптата кожи, взятого из одной папулы, выявлено значительное увеличение количества расширенных и тромбированных сосудов в дерме, демонстрирующих пролиферацию по клубочковому типу. В некоторых сосудах обнаружены укрупнённые клетки со слабобазофильными ядрами и эозинофильной цитоплазмой, которые свободно расположены в просвете кровеносных сосудов (рис. 2). Кроме того, зафиксировано подкожное кровоизлияние. Значительное количество мононуклеарных клеток с периваскулярной и периаднексальной локализацией демонстрировали иммуногистохимическую реакцию на CD68 (KP-1), при этом не экспрессировали общие для лейкоцитов антигены CD3 и CD20 (рис. 3). Часть эндотелиальных клеток экспрессировала антигены CD31 и CD34. Сосуды оказались негативными на белок D2-40.
Рис. 2. Микроскопическое исследование (окрашивание гематоксилином и эозином, ×200): в сосочковом слое дермы определяются эктазированные полнокровные сосуды капиллярного типа с наличием в просвете групп тесно расположенных гистиоцитов с базофильными ядрами и эозинофильной цитоплазмой (стрелки). [Фото из архива РНИМУ им. Н.И. Пирогова. Публикуется впервые с разрешения администрации учреждения].
Fig. 2. Microscopic examination (staining with hematoxylin and eosin, ×200): in the papillary layer of the dermis, ectatized, full-blooded capillary-type vessels are detected with the presence of groups of closely spaced histiocytes with basophilic nuclei and eosinophilic cytoplasm in the lumen (arrows). [Photo from the archive of the Russian National Research Medical University named after N.I. Pirogov. Published for the first time with the permission of the administration of the institution].
Рис. 3. Микроскопическое исследование (окрашивание гематоксилином и эозином, x200): в ретикулярном слое дермы определяются периаднексальные и периваскулярные лимфоцитарные инфильтраты (стрелки). [Фото из архива РНИМУ им. Н.И. Пирогова. Публикуется впервые с разрешения администрации учреждения].
Fig. 3. Microscopic examination (staining with hematoxylin and eosin, x200): periadnexal and perivascular lymphocytic infiltrates are detected in the reticular layer of the dermis (arrows). [Photo from the archive of the Russian National Research Medical University named after N.I. Pirogov. Published for the first time with the permission of the administration of the institution].
Диагноз
На основании клинических данных и результатов гистологического исследования биоптата установлен клинический диагноз: «Внутрисосудистый гистиоцитоз».
Лечение
После постановки диагноза пациентке назначено полное удаление поражённых участков кожи с последующей обработкой швов антисептическим раствором (спиртовой хлоргексидин или Бетадин) и ежедневной сменой повязки. В течение последующих 2–3 дней, находясь в домашних условиях, было предписано обрабатывать повреждённые области кожного покрова до 3–4 раз в сутки без применения повязки.
Исход и прогноз
В результате назначенного лечения достигнуто полное выздоровление без последующего возобновления патологического процесса.
ОБСУЖДЕНИЕ
Внутрисосудистый гистиоцитоз ― малоизученное заболевание, процесс его диагностики специалистами существенно затруднён. Ввиду нечастой встречаемости и неспецифичности симптомов внутрисосудистого гистиоцитоза возникают сложности в процессе постановки верного диагноза и проведения дифференциальной диагностики, что в свою очередь чревато некорректным назначением терапии и усугублением состояния пациента. Примером таких сложностей может служить разобранный нами клинический случай. Дифференциальная диагностика проводилась с целью исключения патологий, имеющих сходные клинические проявления. Результаты дерматоскопии и гистологического исследования биоптата кожи сыграли ключевую роль в подтверждении диагноза внутрисосудистого гистиоцитоза и назначении адекватного лечения. Эти методы исследования позволили выявить характерные изменения сосудистой структуры и клеточной инфильтрации, подтверждающие наличие внутрисосудистого гистиоцитоза.
Одной из особенностей внутрисосудистого гистиоцитоза является его связь с различными инфекционными и системными заболеваниями. В некоторых случаях заболевание развивается на фоне подострого бактериального эндокардита, а также заболеваний сердечно-сосудистой системы, печени и почек [4]. C. Demirkesen и соавт. [1] предположили, что внутрисосудистый гистиоцитоз может служить патогистологическим маркером для более серьёзных состояний, таких как болезнь Крона, саркоидоз, туберкулёз, а также некоторых онкологических заболеваний, однако важно отметить, что в редких случаях внутрисосудистый гистиоцитоз может возникать у соматически здоровых людей [24].
Одной из наиболее часто упоминаемых ассоциаций внутрисосудистого гистиоцитоза является его связь с ревматоидным артритом. C.H. Mensing и соавт. [25] выдвинули гипотезу, что внутрисосудистый гистиоцитоз может представлять собой завершающую стадию реактивного ангиотелиоматоза. Зафиксирован также необычный случай, в котором обострение тонзиллита привело к развитию внутрисосудистого гистиоцитоза, что подчёркивает возможную роль воспалительных процессов в патогенезе заболевания [4].
На сегодняшний день не существует единого стандарта лечения внутрисосудистого гистиоцитоза, что связано с индивидуальными особенностями каждого клинического случая, требующего персонализированного подхода. В медицинской литературе отмечается, что для лечения внутрисосудистого гистиоцитоза могут использоваться препараты стероидного происхождения, обладающие противовоспалительными и иммуномодулирующими свойствами [1, 22], однако их эффективность варьирует в зависимости от формы и стадии заболевания. В случаях вторичного внутрисосудистого гистиоцитоза, вызванного основным заболеванием, успешное лечение базового патологического процесса может привести к улучшению состояния пациента. Например, при ассоциации с ревматоидным артритом положительный эффект может быть достигнут с помощью иммунодепрессантов и антицитокиновой терапии [16].
ЗАКЛЮЧЕНИЕ
Описанный клинический случай имеет особую ценность благодаря своей редкости и уникальности. Такие наблюдения играют ключевую роль в накоплении знаний о внутрисосудистом гистиоцитозе, что позволяет врачам дифференцировать это заболевание от других патологий, имеющих сходные кожные проявления. Способность своевременно распознавать внутрисосудистый гистиоцитоз критически важна, так как от этого зависят корректность лечения и, следовательно, прогноз для пациента.
Одной из главных проблем, связанных с внутрисосудистым гистиоцитозом, остаётся ограниченная информированность медицинского сообщества. Несмотря на описания отдельных случаев, систематизированных данных об этиологии, патогенезе и эффективных методах лечения недостаточно. Продолжение научных исследований в этой области является приоритетной задачей. Особое внимание следует уделять изучению факторов, влияющих на развитие и прогрессирование внутрисосудистого гистиоцитоза. Это позволит не только лучше понимать механизмы заболевания, но и выявлять новые диагностические маркеры, которые помогут врачам быстрее ставить правильный диагноз.
Повышение осведомлённости специалистов, проведение обучающих семинаров и публикация клинических наблюдений способствуют более широкому распространению знаний о внутрисосудистом гистиоцитозе. Достижение этих целей имеет практическое значение: ранняя диагностика позволит своевременно начинать лечение, ориентированное как на устранение самого заболевания, так и на коррекцию связанных патологий, что, в свою очередь, улучшит прогноз для пациентов, увеличив вероятность полного выздоровления или достижения стойкой ремиссии.
ДОПОЛНИТЕЛЬНАЯ ИНФОРМАЦИЯ
Вклад авторов. Д.В. Буланов ― курирование и доработка черновой версии статьи; Ю.С. Подвербная ― сбор литературных источников, подготовка и написание исходного текста статьи. Все авторы одобрили рукопись (версию для публикации), а также согласились нести ответственность за все аспекты работы, гарантируя надлежащее рассмотрение и решение вопросов, связанных с точностью и добросовестностью любой её части.
Согласие на публикацию. Авторы получили письменное информированное добровольное согласие пациента на публикацию персональных данных, в том числе фотографий (с закрытием лица), в научном журнале, включая его электронную версию (дата подписания: 28.10.2024). Объём публикуемых данных с пациентом согласован.
Источники финансирования. Отсутствуют.
Раскрытие интересов. Авторы заявляют об отсутствии отношений, деятельности и интересов за последние три года, связанных с третьими лицами (коммерческими и некоммерческими), интересы которых могут быть затронуты содержанием статьи.
Оригинальность. При создании настоящей работы авторы не использовали ранее опубликованные сведения (текст, иллюстрации, данные).
Доступ к данным. Редакционная политика в отношении совместного использования данных к настоящей работе неприменима, новые данные не собирали и не создавали.
Генеративный искусственный интеллект. При создании настоящей статьи технологии генеративного искусственного интеллекта не использовали.
Рассмотрение и рецензирование. Настоящая работа подана в журнал в инициативном порядке и рассмотрена по обычной процедуре. В рецензировании участвовали два внешних рецензента и научный редактор издания.
ADDITIONAL INFORMATION
Author contributions: D.V. Bulanov, curation and revision of the draft version of the article; Ju.S. Podverbnaya, collection of literary sources, preparation and writing of the original text of the article. Thereby, all authors provided approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Consent for publication: The authors received written informed voluntary consent from the patient to publish personal data, including photographs (with the face covered), in a scientific journal, including its electronic version (date of signing: 28.10.2024). The volume of published data was agreed upon with the patient.
Funding sources: No funding.
Disclosure of interests: The authors have no relationships, activities or interests for the last three years related with for-profit or not-for-profit third parties whose interests may be affected by the content of the article.
Statement of originality: In creating this work, the authors did not use previously published information (text, illustrations, data).
Data availability statement: The editorial policy regarding data sharing does not apply to this work, and no new data was collected or created.
Generative AI: Generative AI technologies were not used for this article creation.
Provenance and peer-review: The present paper was submitted to the journal on a proactive basis and reviewed according to the usual procedure. Two external reviewers and the scientific editor of the publication participated in the review.
About the authors
Dmitriy V. Bulanov
The Russian National Research Medical University named after N.I. Pirogov
Email: dbulanov81@gmail.com
ORCID iD: 0009-0005-3772-6643
SPIN-code: 2641-6658
MD, Cand. Sci. (Medicine), Associate Professor
Russian Federation, MoscowJulia S. Podverbnaya
The Russian National Research Medical University named after N.I. Pirogov
Author for correspondence.
Email: julia_123_julia_123@mail.ru
ORCID iD: 0009-0002-9236-6714
SPIN-code: 1653-2617
Russian Federation, Moscow
References
- Demirkesen C, Kran T, Leblebici C, et al. Intravascular/intralymphatic histiocytosis: A report of 3 cases. Am J Dermatopathol. 2015;37(10):783–789. doi: 10.1097/DAD.0000000000000257
- O’Grady JT, Shahidullah H, Doherty VR, Al-Nafussi A. Intravascular histiocytosis. Histopathology. 1994;24(3):265–268. doi: 10.1111/j.1365-2559.1994.tb00519.x
- Rieger E, Soyer HP, Leboit PE, et al. Reactive angioendotheliomatosis or intravascular histiocytosis? An immunohistochemical and ultrastructural study in two cases of intravascular histiocytic cell proliferation. Br J Dermatol. 1999;140(3):497–504. doi: 10.1046/j.1365-2133.1999.02717.x
- Asagoe K, Torigoe R, Ofuji R, Iwatsuki K. Reactive intravascular histiocytosis associated with tonsillitis. Br J Dermatol. 2006;154(3):560–563. doi: 10.1111/j.1365-2133.2005.07089.x
- Catalina-Fernández I, Alvárez AC, Martin FC, et al. Cutaneous intralymphatic histiocytosis associated with rheumatoid arthritis: Report of a case and review of the literature. Am J Dermatopathol. 2007;29(2):165–168. doi: 10.1097/01.dad.0000251824.09384.46
- Lichtenstein L. Histiocytosis X; integration of eosinophilic granuloma of bone, Letterer-Siwe disease, and Schüller-Christian disease as related manifestations of a single nosologic entity. AMA Arch Pathol. 1953;56(1):84–102.
- Hamre M, Hedberg J, Buckley J, et al. Langerhans cell histiocytosis: An exploratory epidemiologic study of 177 cases. Med Pediatr Oncol. 1997;28(2):92–97. doi: 10.1002/(sici)1096-911x(199702)28:2<92::aid-mpo2>3.0.co;2-n
- McClain K, Jin H, Gresik V, Favara B. Langerhans cell histiocytosis: Lack of a viral etiology. Am J Hematol. 1994;47(1):16–20. doi: 10.1002/ajh.2830470104
- Yu RC, Chu C, Buluwela L, Chu AC. Clonal proliferation of Langerhans cells in Langerhans cell histiocytosis. Lancet. 1994;343(8900):767–768. doi: 10.1016/s0140-6736(94)91842-2
- Lim KP, Milne P, Poidinger M, et al. Circulating CD1c+ myeloid dendritic cells are potential precursors to LCH lesion CD1a+CD207+ cells. Blood Adv. 2020;4(1):87–99. doi: 10.1182/bloodadvances.2019000488
- Badalian-Very G, Vergilio JA, Degar BA, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116(11):1919–1923. doi: 10.1182/blood-2010-04-279083
- Berres ML, Lim KP, Peters T, et al. BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J Exp Med. 2014;211(4):669–683. doi: 10.1084/jem.20130977
- Cui L, Zhang L, Ma HH, et al. Circulating cell-free BRAF V600E during chemotherapy is associated with prognosis of children with Langerhans cell histiocytosis. Haematologica. 2020;105(9):e444–447. doi: 10.3324/haematol.2019.229187
- Okamoto N, Tanioka M, Yamamoto T, et al. Intralymphatic histiocytosis associated with rheumatoid arthritis. Clin Exp Dermatol. 2008;33(4):516–518. doi: 10.1111/j.1365-2230.2008.02735.x
- Requena L, El-Shabrawi-Caelen L, Walsh SN, et al. Intralymphatic histiocytosis. A clinicopathologic study of 16 cases. Am J Dermatopathol. 2009;31(2):140–151. doi: 10.1097/DAD.0b013e3181986cc2
- Abuawad YG, Diniz TA, Kakizaki P, Valente NY. Intravascular histiocytosis: Case report of a rare disease probably associated with silicone breast implant. An Bras Dermatol. 2020;95(3):347–350. doi: 10.1016/j.abd.2019.04.016
- Requena L, Fariña MC, Renedo G, et al. Intravascular and diffuse dermal reactive angioendotheliomatosis secondary to iatrogenic arteriovenous fistulas. J Cutan Pathol. 1999;26(3):159–164. doi: 10.1111/j.1600-0560.1999.tb01822.x
- Rhee DY, Lee DW, Chang SE, et al. Intravascular histiocytosis without rheumatoid arthritis. J Dermatol. 2008;35(10):691–693. doi: 10.1111/j.1346-8138.2008.00544.x
- Aung PP, Ballester LY, Goldberg LJ, Bhawan J. Incidental simultaneous finding of intravascular histiocytosis and reactive angioendotheliomatosis: A case report. Am J Dermatopathol. 2015;37(5):401–404. doi: 10.1097/DAD.0000000000000244
- Takiwaki H, Adachi A, Kohno H, Ogawa Y. Intravascular or intralymphatic histiocytosis associated with rheumatoid arthritis: A report of 4 cases. J Am Acad Dermatol. 2004;50(4):585–590. doi: 10.1016/j.jaad.2003.09.025
- Mazloom SE, Stallings A, Kyei A. Differentiating intralymphatic histiocytosis, intravascular histiocytosis, and subtypes of reactive angioendotheliomatosis: Review of clinical and histologic features of all cases reported to date. Am J Dermatopathol. 2017;39(1):33–39. doi: 10.1097/DAD.0000000000000574
- Nishie W, Sawamura D, Iitoyo M, Shimizu H. Intravascular histiocytosis associated with rheumatoid arthritis. Dermatology. 2008;217(2):144–145. doi: 10.1159/000135630
- Gorlanov IA, Zaslavsky DV, Mineyeva OK, et al. Langerhans cell histiocytosis (histiocytosis X): A case study. Vestnik dermatologii i venerologii. 2013;(1):51–55. EDN: PWLEED
- Bakr F, Webber N, Fassihi H, et al. Primary and secondary intralymphatic histiocytosis. J Am Acad Dermatol. 2014;70(5):927–933. doi: 10.1016/j.jaad.2013.11.024
- Mensing CH, Krengel S, Tronnier M, Wolff HH. Reactive angioendotheliomatosis: Is it ‘intravascular histiocytosis’? J Eur Acad Dermatol Venereol. 2005;19(2):216–219. doi: 10.1111/j.1468-3083.2005.01009.x
Supplementary files