On the issue of diagnosis and treatment of skin pseudolymphoma on the example of a clinical case
- Authors: Olisova O.Y.1, Snarskaya E.S.1, Teplyuk N.P.1, Varshavsky V.A.1, Zolotareva E.S.1, Makhmudi W.1
-
Affiliations:
- The First Sechenov Moscow State Medical University (Sechenov University)
- Issue: Vol 26, No 2 (2023)
- Pages: 105-118
- Section: DERMATO-ONCOLOGY
- Submitted: 11.02.2023
- Accepted: 11.03.2023
- Published: 21.05.2023
- URL: https://rjsvd.com/1560-9588/article/view/217710
- DOI: https://doi.org/10.17816/dv217710
- ID: 217710
Cite item
Abstract
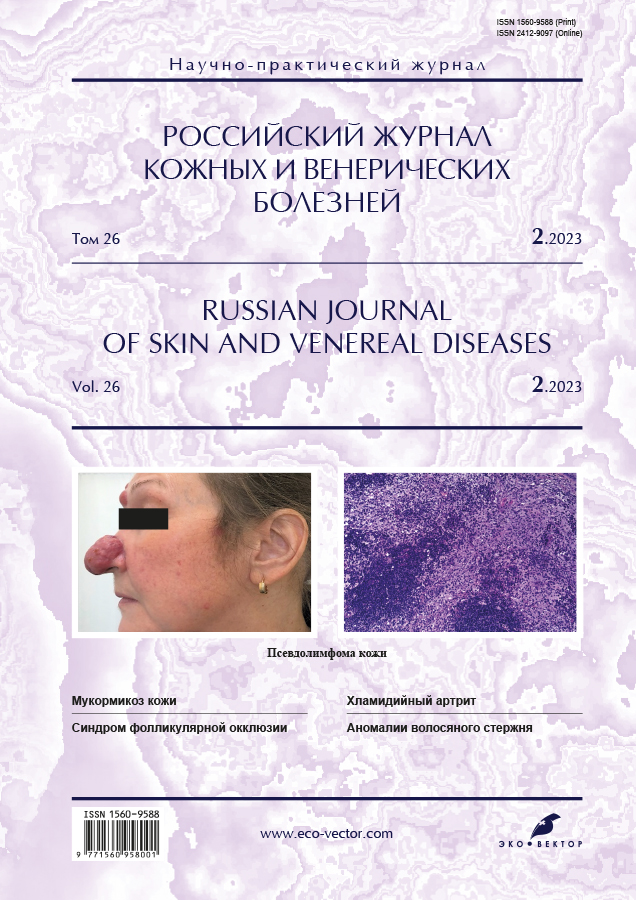
Pseudolymphomas of the skin are a heterogeneous group of diseases manifested by benign lymphoid infiltrates that clinically and/or histologically mimic skin lymphoma.
The group of pseudolymphomas of the skin includes actinic reticuloid, benign lymphocytoma of the skin, true pesvdolymphoma, postscabious lymphoplasia, lymphocytic reactions to insect bites, etc. The diagnosis of pseudolymphoma is based on anamnesis data (the presence of a provoking factor, with the exception of idiopathic pseudolymphomas), clinical picture (a single papule, less often a plaque localized in open areas of the upper half of the body ― the face: cheeks, nose, earlobes; scalp, upper extremities, chest), results histological, immunophenotypic studies, and with persistent persistence of rashes ― on the results of molecular biological studies.
The similarity of clinical and pathomorphological signs of pseudolymph with malignant lymphoproliferative processes creates significant diagnostic difficulties and requires a thorough examination with the involvement of pathologists and oncologists. Diagnostic difficulties are often the cause of erroneous or late detection of skin lymphoma, which negatively affects the prognosis of the disease. Treatment tactics are determined by the morphological variant of lymphoid infiltration, as well as the presence and nature of the provoking factor. The majority of idiopathic psvdolymph is successfully treated with systemic glucocorticosteroids, however, in the case of resistance to systemic glucocorticoids, recommendations on treatment tactics have not yet been developed. Prolonged, often recurrent course, as well as the possibility of transformation of the process into malignant lymphoma of the skin, requires long-term clinical observation of patients.
The case presented in the article confirms that the crucial importance for the successful diagnosis of pseudolymphoma lies in the analysis of anamnesis data, clinical picture, histological and immunohistochemical studies.
Full Text
INTRODUCTION
Pseudolymphoma of the skin (PSL) is a dermatosis caused by lymphoid tissue hyperplasia on a known or unknown factor, of an exogenous or endogenous nature, which has a clinical and / or pathohistological similarity to malignant lymphomas, but differs in a benign course. [6, 8, 9]
Pseudolymphomas are ubiquitous in all races, at all ages, but are more commonly diagnosed in middle-aged and older women. [8] Borrelia-associated pseudo-B-cell lymphoma is common in children and adolescents, while drug-induced pseudo-T-cell lymphoma is more commonly diagnosed in adults. [6, 7]
The etiology of PSL is multifactorial. The spectrum of factors provoking the development of pseudolymphoma, according to foreign and domestic literature, is extremely wide and varied. They can be grouped into three main groups: drugs, foreign antigens, and infectious agents. [1, 2, 5, 11-19] (see table 1)
Table No. 1 Provoking factors for the development of pseudolymphoma
Provoking factors of pseudolymphoma
Medicines Antiarrhythmics (procainamide, mexiletine)
Antibiotics and antimicrobials (penicillin, cefixime, dapsone, nitrofurantoin)
Anticonvulsants (phenytoin, carbamazepine, trimethadione, phenobarbital, primidone, butobarbital, fensuximide)
Anxiolytics (benzodiazepines: clonazepam, lorazepam, triazolam)
Antihistamines (diphenihydramine)
Antidepressants (fluoxetine, doxepin, desipramine, amitriptyline, hydroxybutyrate, lithium carbonate)
Antipsychotics (chlorpromazine, thioridazine, promethazine)
Antirheumatoid drugs (salicylates, allopurinol, D-penicillamine, phenacetin, NSAIDs)
Beta blockers (atenolol, labetalol)
Biologics (tocilizumab, infliximab)
H2 receptor blockers (cimetidine, ranitidine)
Angiotensin II receptor blockers (losartan)
Hypolipidemic (lovastatin)
Diuretics (hydrochlorothiazide, hydrochlorothiazide with amiloride, moduretic)
ACE inhibitors (captopril, enalapril)
Calcium channel inhibitors (verepamil, diltiazem)
Cytostatics (cyclosporine, methotrexate)
Sex hormone preparations (estrogen, progesterone)
Foreign antigens Tattoo pigment, acupuncture, body piercing, silicone implants
Biological antigens Vaccines (hepatitis A, B, diphtheria, tetanus, whooping cough), insect and leech bites
Infectious agents Borrelia burgdoferi, varicella-zoster virus, HIV-infection, Leishmania panamensis, Sarcoptes scabiei.
Of particular interest is the clinical case of PSL development described by Makhecha M. et al. (2019) as a complication after thread facelift using polydioxanone threads. [eleven]
It is also currently suggested that the development of PSL associated with the introduction of some vaccines may be a reaction to the adjuvant (aluminum hydroxide), which is part of many vaccines. [20] However, a case of PSL was later described in a 68-year-old woman 3 months after the second dose of the Pfizer-BioNtech SARS-CoV-2 mRNA vaccine. [21] The development of PSL was preceded by the appearance of an itchy spot at the injection site, while aluminum hydroxide was not included in this vaccine. [21]
Pathogenetic aspects of PSL development
Pseudolymphoma is a reactive process that develops in response to a general or local effect of an irritating factor. [1] When a foreign antigen enters the skin and recognizes it, immune cells of the skin, along with damaged keratinocytes, begin to synthesize pro-inflammatory cytokines (tumor necrosis factor-alpha (TNF-a), interleukins (IL-1a / b, IL-33), stromal lymphopoietin thymus (TSLP), which promote the extravasation of circulating neutrophils, monocytes, and T-lymphocytes [22] Against the background of chronic antigenic stimulation, there is increased migration of lymphocytes through the capillary wall of the superficial vascular plexus of the dermis into the skin, where their activation and proliferation occurs, which is regulated by antiapoptotic the BCL-2 protein found in all lymphoid cells It is classified as an oncogene because damage to the BCL-2 gene has been shown to cause a number of cancers, including skin lymphoma As a result of overexpression of the BCL-2 protein, apoptosis is inhibited, resulting in excessive proliferation of lymphocytes [23]
The appearance of rashes on the skin after a long time after contact with the antigen is explained by the development of a delayed-type hypersensitivity reaction against the background of prolonged exposure to the trigger factor. [22] A clear correlation between the rate of development of the pathological process and the type of provoking factor has not yet been identified. Probably, the reactivity of the process depends to a greater extent on the amount of antigen that has hit the skin and the state of the body's immunity. [2]
Classification
The modern classification of pseudolymphomas is based mainly on the histological and immunohistochemical features of the cellular composition of the skin infiltrate, characterized by the predominance of certain lymphoid cells [1, 2, 4]
There are two main types of cellular infiltrate in pseudolymphomas:
T-cell and B-cell. [1, 2] (see table 2)
Table No. 2 Classification of skin pseudolymphomas
B-cell pseudolymphoma
Benign lymphocytoma of the skin
Borreliosis lymphocytoma
Postherpetic cicatricial lymphocytoma
Postscabious lymphoplasia
Lymphocytoma as a reaction to an insect bite, vaccination, or tattoo pigment
T cell pseudolymphoma
actinic reticuloid
True pseudolymphoma
Lymphocytic infiltration of Jesner-Kanof
Lymphomatoid contact dermatitis
Drug-induced pseudolymphoma
Clinical picture
The group of skin pseudolymphomas includes a wide range of clinical manifestations similar to skin lymphoma, and can manifest as polymorphic rashes in the form of spots, papules, plaques, and even erythroderma. [1, 7]
B-cell pseudolymphoma usually manifests itself as a solitary papule, less often as a solitary plaque, round in shape, with clear boundaries and a smooth surface, sometimes covered with scanty scales, not accompanied by subjective sensations. [1]
For benign lymphocytoma of the skin, localization is characteristic in the face, upper body and on the skin of the upper extremities, while the focus in borreliosis lymphocytoma can be located on the skin of the earlobe, occiput, in the areola of the nipple or scrotum. [2]
The exception is postscabious lymphoplasia and lymphocytoma, which developed after an insect or leech bite, manifested by multiple, widespread, itchy papules at the bite sites, up to the generalization of the process with damage to the entire skin. [1]
Unlike B-cell pseudolymphomas, which are characterized by a relatively similar clinical picture, T-cell pseudolymphomas are a heterogeneous group of diseases with a specific clinical picture for each variant. This group includes:
Actinic reticuloid is an eczematous photodermatitis reaction, occurring mainly in older men and resembling, in severe cases, the eczematous variant of cutaneous T-cell lymphoma. The rashes are represented by itchy, lichenized macules and papules of pink-bluish color, merging with the formation of plaques, and localized in open areas of the skin exposed to chronic insolation: face, neck, dorsal surfaces of the distal extremities. [2] Persistent, persistent itching leads to the appearance of multiple excoriations and serous-hemorrhagic crusts. [1.24]
Lymphocytic infiltration of Yesner-Kanof is manifested by single infiltrated plaques of rounded or irregular outlines, with a smooth surface, localized on the face in the area of the cheeks and cheekbones, neck and upper body, not accompanied by subjective sensations. [1] During the first year, plaque slowly progresses with peripheral growth of lesions and resolution of the central part. The nature of the course of dermatosis is slowly progressive, in the form of peripheral growth of foci and resolution of their central part, with deterioration of the skin process in the autumn-winter period. [1, 2]
True pseudolymphoma has a significant clinical similarity with the initial stages of mycosis fungoides and clinically manifests itself in the form of isolated single or multiple spots of round or oval outlines, pink-red, up to 5 cm in diameter, as well as papules, plaques with scalloped outlines up to 15 cm in size. and / or erythroderma, localized on any part of the skin. The surface of spots, papules and plaques can be smooth or covered with scales, erosions, excoriations, serous and hemorrhagic crusts. The rash is accompanied by persistent, excruciating itching. [1, 2] The erythrodermic variant of lymphomatoid papulosis usually develops in the case of a long course of the disease and is manifested by the fusion of multiple elements with the formation of large cyanotic-purple plaques with scalloped outlines and clear, thickened skin due to pronounced infiltration and increased skin pattern. Vellus hair in the lesions is partially absent, rarefaction of hair in the armpits and on the pubis is possible. Hyperkeratosis of the palms and soles often develops. The skin process may be accompanied by a deterioration in the general condition in the form of subfertile fever, arthralgia, myalgia, generalized lymphadenopathy, sometimes in combination with hepatomegaly. [1] Lymph nodes in the erythrodermic variant are enlarged, painless on palpation, not soldered to each other and to the underlying tissues, of a dense elastic consistency. [1, 4]
Diagnostics
The diagnosis of PSL is based on the combined data of a carefully collected anamnesis, the clinical picture, and the results of histological, immunohistochemical, and molecular studies. [1, 2, 7, 8]
Among the features of clinical and anamnestic data, the presence of long-term persistent localized papules and plaques that are not prone to spread, ulceration, bleeding and/or atrophy, as well as a slowly progressive course of the disease with a tendency to spontaneous regression of elements, are distinguished. A characteristic feature is the asymmetric arrangement of the lesions. In most cases, the causative factor can be identified. [1, 2, 5, 9]
Histological examination in the case of pseudolymphoma reveals a strip-like (diffuse) or focal, clearly defined dense inflammatory lymphoid infiltrate that occurs in the dermis and is delimited from the epidermis by a narrow strip of normal collagen. A band-like infiltrate, located in the upper layers of the dermis, at the border of the papillary and reticular layers, perivascularly and / or perifollicularly, occurs in T-cell pseudolymphomas. While the focal infiltrate characteristic of B-cell pseudolymphomas is more often localized in the reticular layer of the dermis. [1, 9] Polymorphic infiltrate - formed by lymphoid cells and histiocytes, as well as single plasma cells and eosinophils, presented in different ratios with each other. [1] Along with numerous unchanged small lymphocytes, in exceptional cases, large and medium-sized lymphocytes resembling atypical ones are found. [10] The epidermis is intact or slightly altered with signs of acanthosis, spongiosis, hyperkeratosis, or focal parakeratosis, separated from the infiltrate by a narrow strip of unchanged collagen. [4, 8].
Other histological features of pseudolymphoma include the absence of cells with mitosis and apoptosis, the preservation of adnexal skin structures, signs of neoangiogenesis, stromal fibrosis, and the detection of follicle-like structures with germinal centers represented by macrophages. In the presence of germinal centers, it is recommended to determine the expression of CD45RA and BCL-2, pathognomonic for lymphomas. [23]
If the provoking factor could not be identified, and the results of histological examination revealed signs of lymphoma (the infiltrate is located in the deeper layers of the dermis, contains atypical lymphocytes, cells with mitotic patterns), an immunohistochemical study (IHC) based on the detection of CD1a markers is required. , CD3, CD4, CD7, CD8, CD10, CD20, CD21, CD30, CD43, CD56, CD68, CD79a, BCL-2, BCL-6, Ki67 expressed by immunocompetent cells during their differentiation. However, no marker is strictly specific for pseudolymphomas. [4, 7] Detection of polyclonal antigens of lymphocytes using IHC allows to exclude the diagnosis of "lymphoma". [7, 8] When determining clonality by the rearrangement of heavy chains of immunoglobulins (IgH) by polymerase chain reaction (PCR), in the case of pseudolymphoma, polyclonality of the lymphoid population in the blood and skin is detected. [26]
Analysis of the expression of immunoglobulin light chains (IgL) k and λ is recommended in the presence of a questionable histological and immunohistochemical picture. [8] In foreign countries, fluorescent in situ hybridization (FISH) and flow cytometry can be used to isolate light chains. [26] In Russia, the method of immunohistochemical study using paraffin-fixed biopsy material is used. [25] According to its results, in pseudolymphoma, the polyclonal nature of proliferates is distinguished, characterized by the simultaneous expression of both k and λ chains, in a ratio of approximately 2:1 (with k chains predominating in the vast majority of cases). It should be noted that cells of malignant lymphomas produce only one variant of light chains, and more often - type λ. [25]
Additional examination
Laboratory examination, as a rule, does not reveal characteristic changes. In rare cases, eosinophilia, thrombocytopenia, leukocytosis and an increase in ESR are possible. [1] In case of persistent course with frequent relapses or progression of the process, a number of studies are additionally carried out, including trephine biopsy, bone marrow puncture, biopsy of enlarged lymph nodes, CT of the chest, abdominal cavity and small pelvis. [8, 9] If actinic reticuloid is suspected, a photosensitivity test is performed. [3]
Despite modern diagnostic capabilities, patients with pseudolymphomas require long-term follow-up (for at least 5 years) to confirm the benign nature of the process. A repeated comprehensive examination allows you to identify the transformation of a benign process into a malignant one as early as possible. [1]
Differential Diagnosis
Differential diagnosis of PSL presents significant difficulties. Each clinical case requires careful clinical and pathomorphological correlation in order to make the correct diagnosis and select the optimal treatment regimen. [2]
Most often, PSL is differentiated from B-cell lymphoma of the skin, mycosis fungoides, infiltrative forms of sarcoidosis, lupus erythematosus, papular syphilides, Biett's centrifugal erythema. (tables 3 and 4) [2, 8, 9]
Table number 3. Differential diagnosis of B-cell pseudolymphomas with other dermatological diseases
Benign lymphoplasia of the skin
B-cell lymphoma Skin sarcoidosis Papular syphilis Lupus tuberculosis
Gender More women More men Men and women 1:1.1 More men 3:1 More women
Clinical manifestations Solitary papule, less often - a single plaque on the face, earlobe, chest, genitals and extremities. Spots, plaques, nodes with subsequent ulceration and generalization. Papules, plaques, tubercles. Plaques can be single and located on the face, skin of the trunk and extremities. If there are several sarcoid plaques, they are usually located on symmetrical areas of the skin.
Papules Tubercles prone to peripheral growth
Histological picture (morphological features) Acanthosis, upper dermis - polymorphic infiltrate of lymphocytes and histiocytes with an admixture of plasmocytes and eosinophils, single large lymphocytes, vascular proliferation, stromal fibrosis Minimal acanthosis, polymorphic infiltrate of lymphocytes, histiocytes and eosinophils in the deep layers of the dermis, accumulations atypical lymphocytes, lack of fibrosis and vascular proliferation. Sarcoid granuloma in the reticular layer of the dermis or hypodermis The endothelium of the superficial capillaries is swollen, the deep vessels of the dermis are affected, the vessels are surrounded by infiltrate. Tubercles with epithelioid and giant cells and a peripheral zone consisting of lymphocytes.
Provoking factors
Tattoos, herpes simplex virus, prolonged contact with metals, acupuncture, insect bites, leeches, ticks.
Heredity, viral diseases Immune disorders, drugs, substances, bacteria and viruses
Sexual contact Immunodeficiency
The course of the disease
Benign, spontaneous remission Progressive, fatal Chronic, progressive, with possibility of spontaneous remission Under treatment, benign Chronic, progressive
Table number 4. Differential diagnosis of T-cell pseudolymphomas with other dermatological diseases
actinic reticuloid
Jessner-Kanoff lymphocytic infiltration True pseudolymphoma
Mycosis fungoides Bietta centrifugal erythema
Gender More often men More often men Men and women 1:1 Men and women 2:1 More often than women
Clinical manifestations Plaques, papules on the skin of the face Papules and plaques, with clear boundaries and a smooth surface, with a tendency to peripheral growth with simultaneous resolution in the central part of the face (cheeks, forehead).
Spots, papules, plaques, erythroderma. The surface is covered with scales, crusts, excoriations, serous and hemorrhagic crusts. Localization is ubiquitous. Spots, plaques and nodes, erythroderma. Localization of rashes on areas of the skin that are not exposed to solar radiation. Edematous erythema with a smooth surface on the skin of the face.
Histological picture (morphological features) Polymorphic, dense infiltrate, micro-abscesses Potrier Lymphohistiocytic infiltrate with an admixture of plasmocytes around the skin appendages and blood vessels. intact epidermis. Polymorphic, dense infiltrate, "mycotic" cells, weak epidermotropism
Lutzner cells, Potrier microabscesses, consisting of mononuclear elements and Cesari cells, in the Malpighian layer of the epidermis
Focal infiltrate with a tendency to be located around the skin appendages. Hydropic degeneration of the cells of the basal layer of the epidermis.
Provoking factors Contact allergy, photoallergy Diseases of the gastrointestinal tract, insolation, drugs. Drugs, chemicals, foodstuffs Heredity, viral diseases More often insolation, foci of chronic streptococcal infection.
The course of the disease Persistent course with seasonal deterioration in the spring and summer. Remission without treatment is possible with the exclusion of exposure to sunlight. An undulating course with seasonal deterioration in the autumn-winter period and a tendency to spontaneous regression in the summer period. Benign with spontaneous remission Chronic, progressive Rapidly treatable with subsequent recurrence.
Treatment
Treatment of pseudolymphomas, first of all, involves the identification and elimination of a provoking factor, resulting in spontaneous regression of rashes in most cases. [2, 3] Despite this, the use of pathogenetic and symptomatic therapy accelerates the regression of clinical manifestations. In order to eliminate sensitizing agents, both exogenous and endogenous origin, a course of plasmapheresis is recommended. [1.27]
The most effective and common method of treatment is systemic therapy with glucocorticosteroid drugs (GCS). This choice is explained by the possibility of suppressing the body's immune response due to the presence of anti-inflammatory, immunosuppressive and antiproliferative effects. [10] The route of administration of corticosteroids is determined by the severity of pseudolymphoma and the prevalence of rashes. With single rashes, interstitial administration of prolonged glucocorticosteroids (Diprospan) at a rate of 0.5 ml/cm2 is effective. In addition, topical corticosteroids of a strong and very strong class (clobetasol, fluticasone propionate) are used. [1, 10, 28] With widespread rashes, intramuscular injections of betamethasone suspension (Diprospan) 2 ml with a weekly interval are recommended. [1, 10]
Photodynamic therapy is a pathogenetically determined method of pseudolymph therapy and allows selective destruction of pathological cells without damaging surrounding tissues. [37] Case reports of successful use of prednisolone, cyclosporine, rituximab, methotrexate, hydroxychloroquine, oxacillin, mycophenolate mofetil, imiquimod cream, and phototherapy (PUVA) are presented. [1, 29-33]
In case of confirmation of the infectious nature of the provoking factor, it is advisable to conduct etiological therapy. [1, 2] If a borreliosis infection is detected, systemic antibiotics are prescribed for a period of at least three weeks: doxycycline, amoxicillin, or third-generation cephalosporins. [14] Benign lymphoplasia caused by a viral infection is successfully treated with systemic antiviral drugs (acyclovir, famciclovir). [12] Complex therapy of postscabious lymphoplasia includes antiparasitic drugs (scabicides). [1]
To remove foci of lymphoplasia of the skin that has developed at the site of tattoos, fractional laser therapy is used using a carbon dioxide or neodymium laser. [15]
The positive dynamics of the skin process, which is marked by rapid development after the start of anti-inflammatory and detoxification therapy, most likely indicates the benign nature of the pathological process. [1]
Pseudolymphomas are prone to spontaneous regression at various times (from 1 to 32 weeks after the termination of the trigger) and do not affect the quality of life of the patient, however, the development of relapse is possible even after the elimination of the provoking factor. [4]
Here is our clinical observation
Patient O., aged 55, was admitted to the Clinic for Skin and Venereal Diseases. V.A. Rakhmanov with complaints of rashes on the skin of the face, accompanied by moderate soreness and itching.
Disease history:
He considers himself ill since the end of spring 2021, when for no apparent reason rashes appeared on the skin of the face in the area of the brow crease and the tip of the nose, without subjective sensations. The patient associates the onset of the disease with a stressful situation at work and a violation of the diet (she consumed a large amount of chocolate and citrus fruits). Independently used zinc-pyrithione for rashes without a positive effect. She went to a private clinic, where she was diagnosed with "Perioral dermatitis" and prescribed: injections of sodium thiosulfate, topical pimecrolimus cream and ivermectin cream, without a positive effect (according to the patient). In the future, she continued to use zinc-pyrithione on her own with a temporary positive effect in the form of a decrease in the peeling of the surface of the rashes.
In July 2021, she noted the appearance of new rashes on the skin of her right cheek. She did not go to the doctors, she continued to use zinc-pyrithione cream for rashes on her own. A few months later she turned to another private clinic, from where she was sent to the V.A. Rakhmanov to Professor Teplyuk N.P., a preliminary diagnosis of "Pseudolymphoma" was made. At the prehospital stage, in order to clarify the diagnosis, the patient underwent a biopsy under local anesthesia with a 2% lidocaine solution, two sutures and an aseptic dressing were applied. The resulting biopsy was sent for histological and subsequent immunohistochemical studies.
The result of pathomorphological examination:
In skin preparations, the epidermis is pitted, the dermato-epidermal junction is loosened. In the dermis, in all departments, there are pronounced lymphoid infiltrates, mainly perivascular.
Conclusion: the morphological picture fits into pseudolymphoma.
The patient was hospitalized in the clinic of skin and venereal diseases for further examination and therapy.
Local status:
The skin lesion has a chronic subacute inflammatory asymmetric character with localization in the face area. On the skin of the tip of the nose, right cheek, forehead, there are multiple nodes (9 in total) of a rounded shape with a bumpy, shiny surface of a bright pink color with a purple tint. The size of the nodes is different, ranging from 0.5 to 5.5 cm in diameter, they rise above the level of the surrounding tissue. On the surface of some nodes, light brown scales are visible. The largest node, 5.5 x 4.5 cm in size, is located centrofacially at the tip of the nose, occupying a third of its surface; in the area of the right nasolabial fold, there is a slightly smaller node 3.8 x 2.7 cm; 2.6 cm is located in the crease between the eyebrows. Smaller nodes ranging in size from 0.5 to 1.0 cm are located on the skin of the forehead and right neck. (Fig. 1 a, b, c) Such localization of nodes gives the impression of a unilateral process. On palpation, the nodes are painless, densely elastic in consistency, soldered to the surrounding tissue, and not mobile. Skin outside lesions of normal color. Turgor and elasticity correspond to age. Mucous membranes and hair are not affected. The nail plates of the hands and feet are not changed. Lymph nodes are not enlarged. There are no subjective sensations.
Figure 1. (a) Patient N., 43 years old, pseudolymphoma, multiple nodes on the skin of the face.
Figure 1. (b) The same patient. Pseudolymphoma, node on the skin of the nose and forehead (side view), the skin of the left cheek is free from rashes.
Figure 1. (c) The same patient. Pseudolymphoma, multiple nodes on the skin of the right half of the face.
Clinical and laboratory examination:
Complete blood count from 10/19/2021: HCT: 40.8%; HGB: 133 g/l; MCH: 29.1 pg; MCHC: 327 g/l; MCV: 89 fl; PLT: 116 10*9/L; RBC: 4.58 10*12/l; RDW: 13%; WBC: 5 10*9/l; Basophils %: 0.5%; Lymphocytes #: 1.8 10*9/L; Lymphocytes %: 36.6%; Monocytes #: 0.4 10*9/L; Monocytes %: 9%; Neutrophils #: 2.5 10*9/L; Neutrophils %: 50.6%; Unclassifiable %: 2.2%; Unclassifiable quantity: 0.1 10*9/l; ESR Vest.: 13 mm/hour; Color index: 0.87_; Eosinophils #: 0.1 10*9/L; Eosinophils %: 1.1%;
Urinalysis dated 10/19/2021: Bacteria: Not detected; Protein: 0; Bilirubin in urine: Negative; Glucose: Negative; Mushrooms: Not found; Ketone bodies: Detected; Cells of the renal epithelium: Not detected; Quantity: --- ; Blood: - ; Leukocytes: 001; Microscopy: Microscopy; Nitrites: -; Squamous epithelium: Little; Transparency: Transparent; pH reaction: 5.5; Slime: A little; Specific Gravity: 1010 ; Urobilinogen: +3 (140 µmol/L) ; Urine color: Straw yellow; Hyaline cylinders: Not found; Cylinders granular: Not found;
Biochemical blood test dated 10/19/2021: ALT: 16 units/l; Albumin: 41.7 g/l; Amylase: 64 units/l; AST: 20 units/l; Bilirubin total: 13 µmol/l; GGT: 14 U/L; Glucose: 5.29 mmol/l; Iron: 24.7 µmol/l; KA (calc.): 2.54_; Potassium: 4.4 mmol/L; Calcium: 2.34 mmol/l; Creatinine: 99 µmol/l; HDL: 1.6 mmol/l; LDL: 3.7 mmol/l; VLDL: 0.36 mmol/l; Uric acid: 291 µmol/l; Urea: 5.2 mmol/l; Sodium: 140 mmol/l; Total protein: 70.4 g/l; C-reactive protein: 0.99 mg/l; Triglycerides: 0.8 mmol/l; Cholesterol: 5.66 mmol/l; Alkaline phosphatase: 152 U/L;
Coagulogram from 10/19/2021: % of prothrombin according to Quick: 83%; APTT: 1.09 Ratio; INR: 1.15_; Fibrinogen: 3.88 g/l;
Complete blood count from 10/25/2021: HCT: 43.8%; HGB: 140 g/l; MCH: 29.1 pg; MCHC: 320 g/l; MCV: 91 fl; PLT: 117 10*9/L; RBC: 4.81 10*12/l; RDW: 13.2%; WBC: 7.7 10*9/L; Basophils %: 0.4%; Comment: platelets in microclots; Lymphocytes #: 2.2 10*9/L; Lymphocytes %: 28.3%; Monocytes #: 0.8 10*9/L; Monocytes %: 10.6%; Neutrophils #: 4.4 10*9/L; Neutrophils %: 56.5%; Unclassifiable %: 2.3%; Unclassified quantity: 0.2 10*9/l; ESR Vest.: 6 mm/hour; Color index: 0.87_; Eosinophils #: 0.1 10*9/L; Eosinophils %: 1.9%;
Biochemical blood test dated 10/25/2021: ALT: 16 units/l; Albumin: 45 g/l; AST: 14 U/L; Total protein: 73 g/l; Bilirubin total: 7.1 µmol/l; Bilirubin direct: 1.8 µmol/l; GGT: 17 units/l; Glucose: 5.7 mmol/l; Creatinine: 94 µmol/l; CPK: 44 U/l; C-reactive protein: 0.21 mg/l; Triglycerides: 1.05 mmol/L; Cholesterol: 5.11 mmol/l;
Coagulogram from 10/25/2021: % of prothrombin according to Quick: 99%; INR: 1 _; Fibrinogen: 2.92 g/l;
Histological examination of the surgical material of blocks 1-3 from 09/28/2021:
Microscopic description: In skin preparations, the epidermis is thinned, the dermo-epithelial junction is loosened. In the dermis in all layers, pronounced lymphoid infiltrates are predominantly perivascular.
Conclusion: The morphological picture fits into pseudolymphoma.
Rice. 4. (a) Histological preparation. Stained with hematoxylin and eosin; x100. Before treatment. Monomorphic infiltrate, represented by lymphoid cells that are not tropic to the epidermis and form lymphoid-like structures in the middle and deep layers of the dermis.
Comprehensive immunohistochemical study using 4-7 reagents dated 10/04/2021: Microscopic description: In skin preparations, IHC examination revealed: fixation in the cells of infiltrates in the dermis of the following receptors: CD3 +++, CD4++, CD8++, CD20+++. The proliferative activity of the epithelium is moderate.
Conclusion: IHC study confirms the diagnosis of pseudolymphoma.
Rice. 4(b) Immunohistochemical examination of the skin.
Diffuse insignificant CD8+ infiltrate, x100.
Rice. 4(c) Immunohistochemical examination of the skin. Lymphocytes represented by CD20+ form dense lymphoid-like structures, x100.
Rationale for the diagnosis:
Based on the clinical and morphological picture of the disease, the anamnesis data and the nature of the course of the disease, the data of histological and immunohistochemical studies, the diagnosis was made: “Pseudolymphoma of the skin”.
Treatment performed:
The patient was prescribed a complex treatment, including: Diprospan 2 ml interstitial injection of 1-2 ml No. 10 (10/20/21; 10/27/2021); Rovamycin 1.5 million IU, 2 tablets 2 r / day (6 days); Omeprazole 20g 1 caps 2 r / day (10 days); Asparkam 1t 3 r / day (10 days); Fluconazole 250 mg 1 caps 1 r/week (1 day)
External therapy: Pimafucort for rashes 1 r / day.
Against the background of the therapy, there was a positive trend in the form of a gradual regression of rashes. The treatment was well tolerated, without unwanted and side effects. It was recommended to continue the started therapy in full. Monthly regression of rashes by more than 25% of the volume of initial rashes was noted.
Figure 2. (a) Patient N., 43 years old, pseudolymphoma, regression of multiple nodes on the skin of the face. The yellowish hue of the nodes is due to focal fixation of adipocytes.
Figure 2. (b) Patient N., 43 years old, pseudolymphoma, regression of multiple nodes on the skin of the right side of the face.
Figure 2. (c) Patient N., 43 years old, pseudolymphoma, regression of multiple nodes (top view).
Figure 3. (a) Patient N., 43 years old, pseudolymphoma, significant regression of multiple nodes on the skin of the left side of the face.
Figure 3. (b,c) The same patient, significant regression of multiple nodes on the skin of the nose.
Against the background of the therapy, there was a positive trend in the form of plaque flattening and a decrease in the volume of nodes.
Rice. 4 (d) Histological preparation. in the process of treatment. Focal fixation of adipocytes. Monomorphic diffuse scanty lymphoid infiltrate, x100.
CONCLUSION:
None of the methods for diagnosing pseudolymphomas should be evaluated separately from the others. To make a diagnosis, a joint discussion of the results of studies by a pathologist and a dermatologist is required.
Patients with pseudolymphoma should be observed for a long time due to the risk of transformation into malignant skin lymphoma.
The choice of effective management tactics for patients with pseudolymphoma is an urgent problem of modern dermatology. One of the available methods of treatment is intralesional administration of betamethasone propionate, leading to regression of rashes.
About the authors
Olga Yu. Olisova
The First Sechenov Moscow State Medical University (Sechenov University)
Email: olisovaolga@mail.ru
ORCID iD: 0000-0003-2482-1754
SPIN-code: 2500-7989
MD, Dr. Sci. (Med.), Professor, Corresponding Member Russian Academy of Sciences
Russian Federation, 8-2 Trubetskaya street, 119992 MoscowElena S. Snarskaya
The First Sechenov Moscow State Medical University (Sechenov University)
Email: snarskaya-dok@mail.ru
ORCID iD: 0000-0002-7968-7663
SPIN-code: 3785-7859
MD, Dr. Sci. (Med.), Professor
Russian Federation, 8-2 Trubetskaya street, 119992 MoscowNatalya P. Teplyuk
The First Sechenov Moscow State Medical University (Sechenov University)
Email: teplyukn@gmail.com
ORCID iD: 0000-0002-5800-4800
SPIN-code: 8013-3256
MD, Dr. Sci. (Med.), professor
Russian Federation, 8-2 Trubetskaya street, 119992 MoscowVladimir A. Varshavsky
The First Sechenov Moscow State Medical University (Sechenov University)
Email: vavarsh@gmail.com
ORCID iD: 0000-0002-5855-3092
MD, Dr. Sci. (Med.), Proffessor
Russian Federation, 8-2 Trubetskaya street, 119992 MoscowEvgeniya S. Zolotareva
The First Sechenov Moscow State Medical University (Sechenov University)
Email: evgeniyazltrv@gmail.com
ORCID iD: 0000-0002-4086-1740
Clinical Resident of the Department of Skin and Venereal Diseases named after V.A. Rakhmanov
Russian Federation, 8-2 Trubetskaya street, 119992 MoscowWilliam Makhmudi
The First Sechenov Moscow State Medical University (Sechenov University)
Author for correspondence.
Email: dr.williamm@mail.ru
ORCID iD: 0000-0001-6075-411X
Russian Federation, 8-2 Trubetskaya street, 119992 Moscow
References
- Olisova OY, Potekaev NS. Pseudolymphomes of the skin. Moscow: Praktika; 2013. 138 p. (In Russ).
- Dermatooncology. Ed. by G.A. Galil-Ogly, V.A. Molochkov, Yu.V. Sergeev. Moscow: Meditsina dlya vsekh; 2005. P. 577–591. (In Russ).
- Olisova OY. Differential diagnosis of pseudolymph skin with localization on the face. Plastic Sur Cosmetol. 2011;(3):477–481. (In Russ).
- Shetty SK, Hegde U, Jagadish L, Shetty C. Pseudolymphoma versus lymphoma: An important diagnostic decision. J Oral Maxillofac Pathol. 2016;20(2):328. doi: 10.4103/0973-029X.185909
- Hussein MR. Cutaneous pseudolymphomas: Inflammatory reactive proliferations. Expert Rev Hematol. 2013;6(6):713–733. doi: 10.1586/17474086.2013.845000
- Engin B, Songür A, Kutlubay Z, Serdaroğlu S. Lymphocytic infiltrations of face. Clin Dermatol. 2014;32(1):101–108. doi: 10.1016/j.clindermatol.2013.05.031
- Makhecha M, Singh T, Yadav T, Atawane M. Cutaneous pseudolymphoma secondary to facial thread lift procedure. Indian Dermatol Online J. 2019;10(3):322–324. doi: 10.4103/idoj.IDOJ_166_18
- Lewin JM, Farley-Loftus R, Pomeranz MK. Herpes simplex virus-associated pseudolymphoma. Cutis. 2013;92(6):E1–2.
- Sepaskhah M, Yazdanpanah N, Sari AF, Jahromi AM. Cutaneous pseudolymphoma as a rare adverse effect of medicinal leech therapy: A case report and review of the literature. Cureus. 2020;12(4):e7517. doi: 10.7759/cureus.7517
- Maraspin V, Strle F. Borrelial lymphocytoma. Wien Klin Wochenschr. 2022. doi: 10.1007/s00508-022-02064-5
- Kendel M, Toncic RJ, Bradamante M, et al. Dermoscopy of a tattoo pseudolymphoma. Dermatol Pract Concept. 2019;9(1):17–19. doi: 10.5826/dpc.0901a04
- Riyaz N, Sasidharanpillai S, Aravindan KP, et al. Phenytoin induced cutaneous B cell pseudolymphoma. Indian J Dermatol. 2015;60(5):522. doi: 10.4103/0019-5154.164437
- Imafuku S, Ito K, Nakayama J. Cutaneous pseudolymphoma induced by adalimumab and reproduced by infliximab in a patient with arthropathic psoriasis. Br J Dermatol. 2012;166(3):675–678. doi: 10.1111/j.1365-2133.2011.10607.x
- Foley C, Leonard N, Wynne B. Cutaneous pseudolymphoma: A rare side effect of cyclosporine. J Am Acad Dermatol. 2015;72(3):e85–86. doi: 10.1016/j.jaad.2014.09.008
- Kim H, Lim KY, Kang J, et al. Macrophagic myofasciitis and subcutaneous pseudolymphoma caused by aluminium adjuvants. Sci Rep. 2020;10(1):11834. doi: 10.1038/s41598-020-68849-8
- Mintoff D, Scerri L, Betts A. SARS-CoV-2 mRNA vaccine injection site pseudolymphoma. J Eur Acad Dermatol Venereol. 2022;36(1):e20–e22. doi: 10.1111/jdv.17680
- Egawa G, Kabashima K. Role of lymphoid structure in skin immunity. Curr Top Microbiol Immunol. 2020;(426):65–82. doi: 10.1007/82_2020_206
- Ebrahim AS, Sabbagh H, Liddane A, et al. Hematologic malignancies: Newer strategies to counter the BCL-2 protein. J Cancer Res Clin Oncol. 2016;142(9):2013–2022. doi: 10.1007/s00432-016-2144-1
- Aslani SF, Sepaskhah M, Safaei A, Hormozi JS. Cutaneous pseudolymphoma: A clinicopathological study and immunohistochemical patterns. Caspian J Intern Med. 2021;12(3):283–289. doi: 10.22088/cjim.12.3.283
- Sidiropoulos M, Deonizio J, Martinez-Escala ME, et al. Chronic actinic dermatitis/actinic reticuloid: A clinicopathologic and immunohistochemical analysis of 37 cases. Am J Dermatopathol. 2014;36(11):875–881. doi: 10.1097/DAD.0000000000000076
- Tian Z, Shiyu Z, Tao W, et al. Lymphoma or pseudolymphoma: A report of six cases and review of the literature. Dermatol Ther. 2019;32(4):e12807. doi: 10.1111/dth.12807
- Miguel D, Peckruhn M, Elsner P. Treatment of cutaneous pseudolymphoma: A systematic review. Acta Derm Venereol. 2018;98(3):310–317. doi: 10.2340/00015555-2841
- Bailey NG, Elenitoba-Johnson KS. Molecular diagnostics of T-cell lymphoproliferative disorders. Cancer J. 2014;20(1):48–60. doi: 10.1097/PPO.0000000000000016
- Hristov AC, Comfere NI, Vidal CI, Sundram U. Kappa and lambda immunohistochemistry and in situ hybridization in the evaluation of atypical cutaneous lymphoid infiltrates. J Cutan Pathol. 2020;47(11):1103–1110. doi: 10.1111/cup.13858
- Sanchis-Sánchez C, Santos-Alarcón S, Benavente-Villegas FC, et al. Red nodule on the face with “spontaneous” regression. An Bras Dermatol. 2017;92(5 Suppl 1):135–137. doi: 10.1590/abd1806-4841.20175540
- Han B, Liu H, Wang H. A case of multiple nodular cutaneous B-cell pseudolymphoma successfully treated with glucocorticoid, methotrexate, and hydroxychloroquine. Dermatol Ther. 2022:35(11):e15812. doi: 10.1111/dth.15812
- Allison RR, Moghissi K. Photodynamic Therapy (PDT): PDT Mechanisms. Clin Endosc. 2013;46(1):24–29. doi: 10.5946/ce.2013.46.1.24
- Besch-Stokes JG, Patel MH, Brumfiel CM, et al. Cutaneous B cell pseudolymphoma treated with rituximab and methotrexate. Dermatol Online J. 2021;27(9). doi: 10.5070/D327955138
- Balode D, Beļajeva L, Ruesseler V, et al. Diagnostic challenges and treatment options for cutaneous T cell pseudolymphoma: A case study with rituximab treatment. Am J Case Rep. 2020;(21):e919616. doi: 10.12659/AJCR.919616
- Baumgartner-Nielsen J, Lorentzen H. Imiquimod 5%: A successful treatment for pseudolymphoma. Acta Derm Venereol. 2014;94(4):469. doi: 10.2340/00015555-1730
Supplementary files